The idea of the ACGME changes in work hours is that if interns get more sleep and have shorter shifts, there will be improved patient safety and quality of care. Though intuitive, this has never really been proven. The side effect of this proposal is that internship will become "easier"; no longer will interns have war-stories of ridiculously long shifts devoid of sleep. That's a good thing. But in examining my own experience, I think that if I were to redesign the system to improve patient care and help interns, I'd take a different approach.
Currently, inpatient medicine interns admit up to five patients on call. Our personal caps are 10 patients total; each intern cannot be responsible for more than 10 people at one time. The admission cap of five is challenging but acceptable. In a single day (or 24 hour admitting cycle), I can be expected to learn about, talk to, examine, diagnose, and begin treatment for five new patients. When they come all at once, it's overwhelming, but usually I can manage it. However, I have trouble with the personal cap of 10. I know that senior residents and attendings take care of more patients than that, but for an intern who is responsible for all the "scut," 10 patients is a lot. When I'm in the middle of a procedure like a paracentesis, I will get paged over and over about half my other patients. It is not easy each day to see 10 patients, determine their plans, actualize it, and document everything.
I would propose decreasing personal caps simply to nine patients. Though minimal, I think this would decompress the hardest days - those with a full service. I think it'd improve patient care because when I'm running a full service, there are things I want to do for my patients that I don't have time to do. Even having one fewer person means fewer notes, fewer family meetings, fewer calls from pharmacy, fewer nursing pages, fifteen minutes of additional sleep in the morning. It adds up. And by decreasing the overall cap, the experience of residency would not be changed too much, only smoothed at the edges. However, hospitals run on interns, and this would be a burden to the system because more practitioners would be required to account for the same number of beds.
Tuesday, August 31, 2010
Sunday, August 29, 2010
Poem: Untitled
There is a point of strangely prolific writing that happens right at the edge of exhaustion, right when that call of bed intoxicates, and if I resist it a little more, nonsense and happiness come out.
-
There is a great canvas, white and arched
with the pick of the wind, the vibration
of sounding board, the tong-tong-tong
of ideas springing into mist, and dispersed--
Your ideas springing into mist, dispersed
by words, by song and lull, and lullabye,
by quick and row, telltale sound and sense,
turnkey imagined whose golden locks apprehend.
This is fairy tale: this is where I go
where I live, where I talk to myself,
where I fall asleep in a lexicon of arms:
here's a sword, a spear, a halberd;
each word more and more absurd
as I clad myself from the cold. Yes,
this is where I retreat when you lecture me,
when I am wallflowered at a dance I never
meant to be, when I am waiting for a bus,
why I wear no earphones, why I still hear
music in my head; the tong-tong-tong
of grilling drums or giant footsteps
or lavender and brass and dreams awash--
Pickle my words and cast them afloat.
Whichever shores these bits of poems create
make sense, or not, as fairy tales do.
-
There is a great canvas, white and arched
with the pick of the wind, the vibration
of sounding board, the tong-tong-tong
of ideas springing into mist, and dispersed--
Your ideas springing into mist, dispersed
by words, by song and lull, and lullabye,
by quick and row, telltale sound and sense,
turnkey imagined whose golden locks apprehend.
This is fairy tale: this is where I go
where I live, where I talk to myself,
where I fall asleep in a lexicon of arms:
here's a sword, a spear, a halberd;
each word more and more absurd
as I clad myself from the cold. Yes,
this is where I retreat when you lecture me,
when I am wallflowered at a dance I never
meant to be, when I am waiting for a bus,
why I wear no earphones, why I still hear
music in my head; the tong-tong-tong
of grilling drums or giant footsteps
or lavender and brass and dreams awash--
Pickle my words and cast them afloat.
Whichever shores these bits of poems create
make sense, or not, as fairy tales do.
Saturday, August 28, 2010
16
The ACGME is the regulatory body for residency programs, and there are rumors that they will change the work hour limits for next year's incoming residents. The concern is that extended periods of time without sleep put patients at risk. Furthermore, the ACGME is starting to differentiate between first year residents (interns) and senior residents. The proposed change is that interns will be limited to 16 hour shifts. This will effectively change all of internship into shift work such as day teams and night teams with an overlap of an hour or two for patient handoff. Many other limits remain the same: 80 hours a week, one day off a week.
I'm not sure I like this. If the ACGME sets this rule, there's no negotiation, but in my opinion, shift work will take something away from inpatient medicine. There really is something tremendously gratifying and enormously weighty about coming into a 30 hour call, getting very sick patients during the daytime, stabilizing them through night, and going home satisfied the following day. That marathon of a day is what bonds me to my patients and what teaches me real medicine. That being said, many services work well with day and night shift work. For example, I thought shift work was perfect for labor and delivery; the main reason for admission to the hospital ("I'm having a baby") is generally straightforward so the patient handoffs between the day and night teams aren't difficult. Furthermore, patients appreciate similar faces each day and night. It's harder for patients to understand the concept of "call."
It seems as though we will move to the 16 hour rule and shift work, and programs are really trying to address that. At UCSF, one hospital is running both the traditional system alongside a proposed system for next year to iron out problems. At Stanford, committees are forming to figure out staffing needs. Hospitals as a whole may need to find resources to hire more hospitalists or nocturnists (staff physicians at night) and programs need to figure out how to maintain educational didactics when some residents will be on during the daytime and some at night. Lots of change will happen within the next few years.
I'm not sure I like this. If the ACGME sets this rule, there's no negotiation, but in my opinion, shift work will take something away from inpatient medicine. There really is something tremendously gratifying and enormously weighty about coming into a 30 hour call, getting very sick patients during the daytime, stabilizing them through night, and going home satisfied the following day. That marathon of a day is what bonds me to my patients and what teaches me real medicine. That being said, many services work well with day and night shift work. For example, I thought shift work was perfect for labor and delivery; the main reason for admission to the hospital ("I'm having a baby") is generally straightforward so the patient handoffs between the day and night teams aren't difficult. Furthermore, patients appreciate similar faces each day and night. It's harder for patients to understand the concept of "call."
It seems as though we will move to the 16 hour rule and shift work, and programs are really trying to address that. At UCSF, one hospital is running both the traditional system alongside a proposed system for next year to iron out problems. At Stanford, committees are forming to figure out staffing needs. Hospitals as a whole may need to find resources to hire more hospitalists or nocturnists (staff physicians at night) and programs need to figure out how to maintain educational didactics when some residents will be on during the daytime and some at night. Lots of change will happen within the next few years.
Friday, August 27, 2010
80
Eighty is the other limit. We cannot work more than eighty hours a week. Which is odd because to some people it seems like so much, and yet now that I am here, I realize it's really easy to hit eighty. No problem at all. It is interesting because the 80 hour work week was conjured up from nowhere; a committee sat down and picked an arbitrary number. Is it too much? Too little? I'm not sure; but I can tell you without doubt that 80 hours is not enough time for me to be the kind of doctor I want to be. And yet at the same time, 80 hours is fiercely exhausting.
Wednesday, August 25, 2010
30
Thirty is the magic number this year. Our shifts are limited to 30 hours in length. Is that too much? Is that too little? That's the big debate for next year (which will be an upcoming post). For me, at least, 30 is pretty much the limit. If I don't get any sleep (or even if I get an hour or two), the clarity of my thinking, my response time, my memory all diminish after rounding hour 24. I take so much longer to finish notes, to make clinical decisions, to communicate my thoughts. And beyond hour 30, I really don't think it's appropriate for me to have primary patient care responsibilities.
That being said, 30 is an arbitrary number. Patients aren't nicely packaged by hour 30 for me to hand off to the next resident. Families are arriving, big decisions are happening, consulting teams are weighing in. It's really not ideal to have a hand-off on the second day of hospitalization, but hour 30 falls right in the middle of it. It will be interesting to see how things change over time.
That being said, 30 is an arbitrary number. Patients aren't nicely packaged by hour 30 for me to hand off to the next resident. Families are arriving, big decisions are happening, consulting teams are weighing in. It's really not ideal to have a hand-off on the second day of hospitalization, but hour 30 falls right in the middle of it. It will be interesting to see how things change over time.
Tuesday, August 24, 2010
Sleep
Sleep has really become a luxury and premium. There is so much I could write about it, but all my thoughts are scattered. I get a generous amount of sleep each night, but I think I get behind when I'm on call. Call can be brutal; we go in expecting to stay awake 30 hours (and then drive home afterward). Even if we do get that precious two or three hours of rest, it is constantly interrupted by pages, fraught with the stress of patient care, and unfulfilling given the furniture provided. I was told to try to get at least an hour because it makes the post-call day so much easier, and it's true. But I would never call it an hour of restful sleep; it's merely an attempt to stave off exhaustion.
As I tread into my third (out of five) straight call months, I can easily say that I am more tired than I have ever been. I crave sleep so, so much, and it's hard for me to remember what it's like not to be exhausted. Sleep is slowly overtaking everything in terms of priority; I know I have calls to return, emails to write, an apartment to clean, a future to plan, and each day I procrastinate a little more. I need to take one of my coveted days off simply to catch up on everything: blogs, correspondence, chores, errands, and sleep. This is a strange, strange life, and I'm not sure how many people know what it's like before they get into it.
I know I've been writing several self-pitying blogs, but I'm really going to get out of this rut, I promise.
As I tread into my third (out of five) straight call months, I can easily say that I am more tired than I have ever been. I crave sleep so, so much, and it's hard for me to remember what it's like not to be exhausted. Sleep is slowly overtaking everything in terms of priority; I know I have calls to return, emails to write, an apartment to clean, a future to plan, and each day I procrastinate a little more. I need to take one of my coveted days off simply to catch up on everything: blogs, correspondence, chores, errands, and sleep. This is a strange, strange life, and I'm not sure how many people know what it's like before they get into it.
I know I've been writing several self-pitying blogs, but I'm really going to get out of this rut, I promise.
Monday, August 23, 2010
Taking Care of Ourselves
There is some irony that I spend the majority of my time taking care of other people yet I take awful care of myself. To be honest, residency is the least healthy I've ever been. I feel completely wiped out. I'm not eating well. I'm snacking on junk food and fast food to my great shame - and yet I can find no time to make it to a supermarket to get fruits and vegetables. I'm not exercising, except for pacing up and down the hallways and racing up the stairs when elevators frustrate me. I don't sleep enough. I'm chronically fatigued, yet I can't help it. Looking at my peers, we're all like this. We're losing years of our life as we find ourselves cornered into this situation where convenience outstrips health. I don't even have time to cut my nails. Residency is a very odd beast, and I can see why medicine engenders this feeling that I am sacrificing myself for others - even though I really should not be.
Saturday, August 21, 2010
Still No Sleep
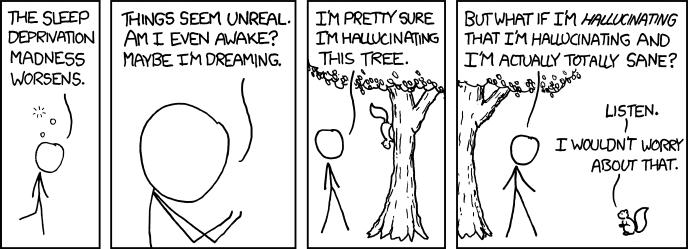 Image from xkcd.com, drawn by Randall Munroe, shown under Creative Commons Attribution-NonCommercial 2.5 License.
Image from xkcd.com, drawn by Randall Munroe, shown under Creative Commons Attribution-NonCommercial 2.5 License.
Friday, August 20, 2010
Possession
With intern year comes an interesting phenomenon: ownership of my patients. My patients identify me as their primary doctor, and I get attached to them. All the medical decisions that happen to my patients ought to go through me, and although much of the time, their plan of care is dictated by my resident or attending, I am the one who does the grunt work making it happen. As a result, interns become very protective of our patients. It is a wonderful and fulfilling role to play, and one that justifies the ridiculous hours we work.
Wednesday, August 18, 2010
Cross-Cover
There is no doubt in my mind that cross-cover is the worst thing ever. It's awful. Cross-covering means that when I am on call, as my co-interns (bless their hearts) finish up their work-day, they sign out their patients to me. If the interns have clinic in the afternoon, we start taking responsibility for their patients at around noon; otherwise, we get sign-outs from 4-6pm. We hold these until night float comes at 10pm.
The problem with cross-covering is that we don't know the patients well. Even with a good sign-out of pertinent medical problems, I end up caring for up to 40 patients (usually and thankfully it averages about half of that), and I have this while trying to admit new patients to my service. Theoretically, cross-covering should be minimal. Most of the work during the daytime should be done for these patients, but the truth is, cross-covering can become the worst nightmare. There are the annoying unimportant calls about medications that have to be renewed or itching or "just wanted to check to see what the plan is, doctor." These can get really frustrating because they constantly interrupt us while we're seeing new patients.
But not infrequently, an unanticipated serious problem comes up: chest pain, seizure, shortness of breath, tachycardia, hypotension. Upon seeing the patient, I'm occasionally alarmed by how sick they look or how fast they seem to be deteriorating. Then, there's a scramble to get more help, learn as much as I can about the patient, and prevent him from getting much worse. I've had cross-cover duties tie my hands for hours as I try to resuscitate someone I don't know well.
Unfortunately, there's no great way around cross-covering; it's such a blessing when I'm not on call and I can leave at 4. But I also cringe when I find out that my cointerns were called on my patients, especially if it was unanticipated or unnecessary. The best moment of my call nights are around 10pm when the night float comes and takes away all those sign-outs to let me concentrate on my own patients who I might have neglected as I found myself spread too thin.
Along those lines, I'm still at the hospital, mostly because I'm less distracted here, but also to hold my pager a little longer and prevent one or two unnecessary pages to my co-intern who will be cross-covering my patients tonight.
The problem with cross-covering is that we don't know the patients well. Even with a good sign-out of pertinent medical problems, I end up caring for up to 40 patients (usually and thankfully it averages about half of that), and I have this while trying to admit new patients to my service. Theoretically, cross-covering should be minimal. Most of the work during the daytime should be done for these patients, but the truth is, cross-covering can become the worst nightmare. There are the annoying unimportant calls about medications that have to be renewed or itching or "just wanted to check to see what the plan is, doctor." These can get really frustrating because they constantly interrupt us while we're seeing new patients.
But not infrequently, an unanticipated serious problem comes up: chest pain, seizure, shortness of breath, tachycardia, hypotension. Upon seeing the patient, I'm occasionally alarmed by how sick they look or how fast they seem to be deteriorating. Then, there's a scramble to get more help, learn as much as I can about the patient, and prevent him from getting much worse. I've had cross-cover duties tie my hands for hours as I try to resuscitate someone I don't know well.
Unfortunately, there's no great way around cross-covering; it's such a blessing when I'm not on call and I can leave at 4. But I also cringe when I find out that my cointerns were called on my patients, especially if it was unanticipated or unnecessary. The best moment of my call nights are around 10pm when the night float comes and takes away all those sign-outs to let me concentrate on my own patients who I might have neglected as I found myself spread too thin.
Along those lines, I'm still at the hospital, mostly because I'm less distracted here, but also to hold my pager a little longer and prevent one or two unnecessary pages to my co-intern who will be cross-covering my patients tonight.
Tuesday, August 17, 2010
VA Wards
I guess now that I am finishing up my second month, I should write about it. After ICU, I went to wards at the VA. Medicine wards form the foundation for the internal medicine internship year. I once heard that the hospital runs on interns, and here it is true. There are five teams, and in each team, there are two interns, a resident, and often a gaggle of medical students. Each intern takes responsibility for up to ten patients, and each call night (every five days), the interns take up to six new patients. It runs in a pretty standard fashion, similar to the way UCSF operated. Each day, I arrive at around 7 to get sign-out on my patients overnight. I see them all, then work-round with the resident to get all the details squared away. Morning report is at 10, and after that, we have attending rounds to staff all the patients. During the afternoon, I get "work" done: notes, studies, discharges, consults.
On call days, we stay overnight admitting patients. Most patients come in through the ED, though we often get a few ICU transfers as well. As an intern, I work more independently than I did as a medical student, trying to come up with a diagnosis and plan myself. We admit until 2am (or until we cap at 6 new patients each), then tuck the patients in until the morning. During the morning, we staff all the new patients with the attending and a day float resident. The day float resident stays during the post-call day as we scramble to get home by the 30 hour rule. It's a pretty standard structure.
On call days, we stay overnight admitting patients. Most patients come in through the ED, though we often get a few ICU transfers as well. As an intern, I work more independently than I did as a medical student, trying to come up with a diagnosis and plan myself. We admit until 2am (or until we cap at 6 new patients each), then tuck the patients in until the morning. During the morning, we staff all the new patients with the attending and a day float resident. The day float resident stays during the post-call day as we scramble to get home by the 30 hour rule. It's a pretty standard structure.
Saturday, August 14, 2010
Anemia II
This is a continuation of the previous post (scroll down). A quick apology for the delayed blogs - I always seem to exceed my self-allotted time for writing.
With regards to the longstanding anemia, this 80 year old woman had repeatedly declined colonoscopy. She understood the risks and benefits - and our suspicion that her anemia was due to colorectal cancer - yet still declined. She didn't have incredibly persuasive reasoning, just that she didn't want it. She said that her parents died of old age, and she wanted to die of old age as well - a feat that is incredibly hard to do in today's era of modern medicine. "As long as I'm not in pain, I'm fine. I don't need to know why my blood counts are low. I just want you to give me my transfusion and send me on my way."
Most medical practitioners would not be comfortable with such a statement. For us, why someone has anemia is fundamentally important. After all, transfusions are not a risk-free or cheap intervention and if we can prevent the anemia, then we can eliminate the need for transfusion. Furthermore, our suspicion was high for cancer and as doctors, we want to find out and intervene. Cancer is one of those things that gets our hearts going; we need to get it before its too late.
During this hospitalization, I again offered colonoscopy, and she again declined. But when on physical exam I found a large spleen, I told her that we would like to do an abdominal ultrasound. I would like to say I offered this to her, but you know how doctors (even second month residents) can be: I probably said, "You feel this mass in your belly, right? We'd like to take a picture of it with an ultrasound machine - similar to the kind they use in pregnancy. It won't hurt. That's okay, right?" Certainly, she could have said no, but I didn't dwell too long on it - after all, an ultrasound is minimally invasive.
The ultrasound found spleen and liver masses. A CT followed, then a PET scan, until we were at a real crossroads. We wanted a biopsy; we wanted tissue. Was this lymphoma? Metastatic carcinoma? Disseminated infection? Something else? But she - and I expected this from talking to her - simply wanted to go home. She had received her transfusions and felt better. As far as she was concerned, our care was excellent but overboard. She never really asked for all the imaging studies and was nonplussed by what we found.
"I'm not in pain. You say there are these lesions in the liver and spleen, and that's fine. They're not bothering me. I'd like to go home. I want to play my clarinet. I want to be with my grandsons. I'm feeling perfect after those transfusions. Thank you." We pressed her. "Yes," she said, "I know you think it is cancer. I know it'll probably kill me. I'm 80. I'm okay with that."
So we sent her on her way with an appointment with her primary care doctor to follow up on this potential malignancy. But the resident and I had our reservations. Had we done too much? Did she really need that ultrasound and CT and PET? All of the things we were doing were things we wanted to do, but were they really consistent with her goals of care?
To be honest, I felt that we hadn't been completely ethically sound there. Of course, we cannot force anyone to do anything they don't want to do, and we hadn't here. But doctors are very skewed creatures. We're biased. We see an abnormal finding, and we want to know what it is. We need to know if we can treat it, even if that involves toxic chemotherapy. And when a patient tells us she wants to die of old age and doesn't need to know, it clashes with our frame of reference. We start wondering whether the patient is really competent and then labeling them as "difficult."
But here, the patient was completely right. Her goals with regard to health care were simple: keep me symptom free. Do no harm. Whatever she has will kill her. She's okay not knowing. She's okay dying of "old age." We not only have to accept that but support her wholeheartedly in attaining that goal.
With regards to the longstanding anemia, this 80 year old woman had repeatedly declined colonoscopy. She understood the risks and benefits - and our suspicion that her anemia was due to colorectal cancer - yet still declined. She didn't have incredibly persuasive reasoning, just that she didn't want it. She said that her parents died of old age, and she wanted to die of old age as well - a feat that is incredibly hard to do in today's era of modern medicine. "As long as I'm not in pain, I'm fine. I don't need to know why my blood counts are low. I just want you to give me my transfusion and send me on my way."
Most medical practitioners would not be comfortable with such a statement. For us, why someone has anemia is fundamentally important. After all, transfusions are not a risk-free or cheap intervention and if we can prevent the anemia, then we can eliminate the need for transfusion. Furthermore, our suspicion was high for cancer and as doctors, we want to find out and intervene. Cancer is one of those things that gets our hearts going; we need to get it before its too late.
During this hospitalization, I again offered colonoscopy, and she again declined. But when on physical exam I found a large spleen, I told her that we would like to do an abdominal ultrasound. I would like to say I offered this to her, but you know how doctors (even second month residents) can be: I probably said, "You feel this mass in your belly, right? We'd like to take a picture of it with an ultrasound machine - similar to the kind they use in pregnancy. It won't hurt. That's okay, right?" Certainly, she could have said no, but I didn't dwell too long on it - after all, an ultrasound is minimally invasive.
The ultrasound found spleen and liver masses. A CT followed, then a PET scan, until we were at a real crossroads. We wanted a biopsy; we wanted tissue. Was this lymphoma? Metastatic carcinoma? Disseminated infection? Something else? But she - and I expected this from talking to her - simply wanted to go home. She had received her transfusions and felt better. As far as she was concerned, our care was excellent but overboard. She never really asked for all the imaging studies and was nonplussed by what we found.
"I'm not in pain. You say there are these lesions in the liver and spleen, and that's fine. They're not bothering me. I'd like to go home. I want to play my clarinet. I want to be with my grandsons. I'm feeling perfect after those transfusions. Thank you." We pressed her. "Yes," she said, "I know you think it is cancer. I know it'll probably kill me. I'm 80. I'm okay with that."
So we sent her on her way with an appointment with her primary care doctor to follow up on this potential malignancy. But the resident and I had our reservations. Had we done too much? Did she really need that ultrasound and CT and PET? All of the things we were doing were things we wanted to do, but were they really consistent with her goals of care?
To be honest, I felt that we hadn't been completely ethically sound there. Of course, we cannot force anyone to do anything they don't want to do, and we hadn't here. But doctors are very skewed creatures. We're biased. We see an abnormal finding, and we want to know what it is. We need to know if we can treat it, even if that involves toxic chemotherapy. And when a patient tells us she wants to die of old age and doesn't need to know, it clashes with our frame of reference. We start wondering whether the patient is really competent and then labeling them as "difficult."
But here, the patient was completely right. Her goals with regard to health care were simple: keep me symptom free. Do no harm. Whatever she has will kill her. She's okay not knowing. She's okay dying of "old age." We not only have to accept that but support her wholeheartedly in attaining that goal.
Thursday, August 12, 2010
Anemia I
Details of this story have been changed. This is about a patient I had on call on medicine wards (which I know I haven't really written about - I'm behind in all the things I want to say). There will be two posts. Today I will introduce the clinical case and ruminate on pre-test probability (one of my favorite topics, I know). Tomorrow, I will discuss an ethical situation I encountered.
An 80 year old woman presents with severe anemia. While a normal hemoglobin might be 12-15 (normal hematocrit 35-45), her hemoglobin was 5 (hematocrit 15). This was one of the lowest I'd ever seen. She presented with shortness of breath and dizziness on exertion as you would expect. She was otherwise completely asymptomatic. If you or I suddenly dropped our hemoglobin to 5, we would be dead. But her anemia had been going on for several years, and her body adapted to it. As an outpatient, she had gotten some blood tests to sort it out: she had an MCV of 81, a low serum iron, high ferritin, low transferrin, low TIBC, poor reticulocytosis. Her peripheral smear showed a bit of everything except schistocytes: she had some polychromasia, anisocytosis, poikilocytosis, ovalocytes, basophilic stippling - nothing too diagnostic. Her vitamin B12 and folate were low-normal. As an outpatient, she had been started on iron and B12 but her anemia continued to worsen; over the course of three years, she dropped her hemoglobin from 12 to 5.
Certainly, if you looked at her numbers, she appeared to have an anemia of chronic disease. However, she simply did not look like someone with a chronic autoimmune disease or indolent infection or cancer. She was active; she played the piano, she walked a mile a day (though more recently, has needed to stop and rest), she worked at a post office. Her past medical history was unremarkable; she had a mastectomy and some high blood pressure. She just took hydrochlorothiazide. She denied drugs and smoking. She occasionally drank alcohol. Overall, she was doing pretty well; she just didn't seem sick.
If you were going to play odds, anemia in an 80 year old is colon cancer until proven otherwise. She had some fecal occult blood tests and 1/3 were positive. She had a sigmoidoscopy over 10 years ago and has been declining colonoscopy since. At each visit with her primary care doctor they discuss the need for colon cancer screening, and each time she politely declines. She's even declined blood transfusions in the past as her symptoms are quite minimal. She just didn't want to go to the hospital.
We admitted her to give her some blood. Easy admission, I thought to myself. (Famous last words). I went to go see her; she was incredibly pleasant and talkative, not short of breath even with that dramatic anemia. Her vital signs were normal. She had a systolic ejection murmur heard throughout the precordium. Otherwise, I thought her initial exam was benign.
I sat down to write my note. It was two or three in the morning. I rubbed my eyes. I got to my problem list: #Anemia, I wrote. When I first started my clinical years, I thought it was weird that doctors would do this "pound" thing.
#Anemia
#Hypertension
#Elevated Creatinine
#FEN
#Dispo
#Code Status
I always thought it was just lazy; wouldn't it look better and be nicer to actually number them? But then I became inculcated into this odd nomenclature and do it myself. I guess new problems pop up and old ones disappear and problems change in priority (which affects the order) and renumbering everything each day is simply a waste of time.
#Anemia, I wrote. What a great internal medicine problem. I decided to actually write a decent note (plus, I had a medical student following me and that prompts me to write better notes to set a good example). I outlined my way of thinking of anemia. I started trying to tease out the cause of her anemia. When I first heard of her, I sort of dismissed it as "probably colon cancer, but we won't find out since she declines colonoscopy." But the more I thought of it, the weirder the case became. She had low platelets for no clear reason and an elevated white blood cell count without evidence of infection. She had a dissociation between her albumin and total protein. Her renal function was worse than I'd expected.
Trying to depuzzle something at 3 in the morning is always a challenge, but I realized she might have something else going on. My suspicion was heightened - even if common things are common, I should at least entertain the idea of a bone marrow problem like myelodysplastic syndrome or even leukemia. And the way I connected kidneys to anemia was with multiple myeloma.
When I went back to examine her in the morning (two hours later), I paid much closer attention to her lymph nodes and abdominal exam. Whoa. I found something. Her spleen was 4 cm below her costal margin (below the ribcage). Normally, I can't feel a spleen at all. Indeed, I had written that her belly examination the night before was "normal." I was a little embarrassed, but you find what you're looking for. When my pre-test probability for an abnormality was a little higher, I convinced myself much quicker that I had an abnormal exam. It also reminded me cursory examinations are not acceptable. More on the workup tomorrow.
An 80 year old woman presents with severe anemia. While a normal hemoglobin might be 12-15 (normal hematocrit 35-45), her hemoglobin was 5 (hematocrit 15). This was one of the lowest I'd ever seen. She presented with shortness of breath and dizziness on exertion as you would expect. She was otherwise completely asymptomatic. If you or I suddenly dropped our hemoglobin to 5, we would be dead. But her anemia had been going on for several years, and her body adapted to it. As an outpatient, she had gotten some blood tests to sort it out: she had an MCV of 81, a low serum iron, high ferritin, low transferrin, low TIBC, poor reticulocytosis. Her peripheral smear showed a bit of everything except schistocytes: she had some polychromasia, anisocytosis, poikilocytosis, ovalocytes, basophilic stippling - nothing too diagnostic. Her vitamin B12 and folate were low-normal. As an outpatient, she had been started on iron and B12 but her anemia continued to worsen; over the course of three years, she dropped her hemoglobin from 12 to 5.
Certainly, if you looked at her numbers, she appeared to have an anemia of chronic disease. However, she simply did not look like someone with a chronic autoimmune disease or indolent infection or cancer. She was active; she played the piano, she walked a mile a day (though more recently, has needed to stop and rest), she worked at a post office. Her past medical history was unremarkable; she had a mastectomy and some high blood pressure. She just took hydrochlorothiazide. She denied drugs and smoking. She occasionally drank alcohol. Overall, she was doing pretty well; she just didn't seem sick.
If you were going to play odds, anemia in an 80 year old is colon cancer until proven otherwise. She had some fecal occult blood tests and 1/3 were positive. She had a sigmoidoscopy over 10 years ago and has been declining colonoscopy since. At each visit with her primary care doctor they discuss the need for colon cancer screening, and each time she politely declines. She's even declined blood transfusions in the past as her symptoms are quite minimal. She just didn't want to go to the hospital.
We admitted her to give her some blood. Easy admission, I thought to myself. (Famous last words). I went to go see her; she was incredibly pleasant and talkative, not short of breath even with that dramatic anemia. Her vital signs were normal. She had a systolic ejection murmur heard throughout the precordium. Otherwise, I thought her initial exam was benign.
I sat down to write my note. It was two or three in the morning. I rubbed my eyes. I got to my problem list: #Anemia, I wrote. When I first started my clinical years, I thought it was weird that doctors would do this "pound" thing.
#Anemia
#Hypertension
#Elevated Creatinine
#FEN
#Dispo
#Code Status
I always thought it was just lazy; wouldn't it look better and be nicer to actually number them? But then I became inculcated into this odd nomenclature and do it myself. I guess new problems pop up and old ones disappear and problems change in priority (which affects the order) and renumbering everything each day is simply a waste of time.
#Anemia, I wrote. What a great internal medicine problem. I decided to actually write a decent note (plus, I had a medical student following me and that prompts me to write better notes to set a good example). I outlined my way of thinking of anemia. I started trying to tease out the cause of her anemia. When I first heard of her, I sort of dismissed it as "probably colon cancer, but we won't find out since she declines colonoscopy." But the more I thought of it, the weirder the case became. She had low platelets for no clear reason and an elevated white blood cell count without evidence of infection. She had a dissociation between her albumin and total protein. Her renal function was worse than I'd expected.
Trying to depuzzle something at 3 in the morning is always a challenge, but I realized she might have something else going on. My suspicion was heightened - even if common things are common, I should at least entertain the idea of a bone marrow problem like myelodysplastic syndrome or even leukemia. And the way I connected kidneys to anemia was with multiple myeloma.
When I went back to examine her in the morning (two hours later), I paid much closer attention to her lymph nodes and abdominal exam. Whoa. I found something. Her spleen was 4 cm below her costal margin (below the ribcage). Normally, I can't feel a spleen at all. Indeed, I had written that her belly examination the night before was "normal." I was a little embarrassed, but you find what you're looking for. When my pre-test probability for an abnormality was a little higher, I convinced myself much quicker that I had an abnormal exam. It also reminded me cursory examinations are not acceptable. More on the workup tomorrow.
Tuesday, August 10, 2010
Healthcare as a Right
With the passage of the recent healthcare bill, I've started thinking what makes healthcare a right? Certainly, like many of my classmates, I believe this, but what makes it true? Is it an inherent property of being human or living in a society that we deserve to be seen by a doctor when we are sick? Or is healthcare really a function of individual wealth or societal wealth?
For me, the answer actually comes from political philosopher John Rawls. "Justice," he writes, "is the first virtue of social institutions, as truth is of systems of thought. A theory however elegant and economical must be rejected or revised if it is untrue; likewise laws and institutions no matter how efficient and well-arranged must be reformed or abolished if they are unjust. Each person possesses an inviolability founded on justice that even the welfare of society as a whole cannot override."
In the same way, care of the patient is the first virtue of the physician. To a physician, reimbursement, lifestyle, respect, sense of self-worth are all secondary endpoints, and a physician who values these things higher than the patient's care is not a physician at all. The undertaking of medicine necessarily involves sacrifice on the part of the doctor, a setting aside of his own priorities to take on that of the patient, and this is fundamental to the development of trust between the patient and physician that must happen for healing to occur. A patient who does not trust his doctor guts his doctor of the tools of his trade, and a patient cannot trust his doctor unless he knows his doctor prioritizes his care over his own selfish ends.
Furthermore, this ordering of priorities is mandated regardless of who the patient is. The physician must care for and value higher than himself any patient who comes before him; he cannot pick and choose. In the same way that a theory must be dismantled if false or a government must be abolished if unjust, a physician cannot be a physician if he selects who he sees or what he does on the basis of money or insurance.
We are morally obligated to place the patient before ourselves; this is the patient-physician covenant. And as a result, insurance status ought not to influence who we treat. This is an external factor that arises in this ridiculous milieu we call healthcare delivery, and by ridding ourselves of its constraints, we rid ourselves of inadvertently discriminating against the uninsured when this has no bearing on who we treat. We must demand a forum of equality for patients to see doctors; we cannot bar them at the door. This is why healthcare equality - and in this instance, universal insurance - is so important. It allows doctors to do their job, that is, put patients before themselves.
For me, the answer actually comes from political philosopher John Rawls. "Justice," he writes, "is the first virtue of social institutions, as truth is of systems of thought. A theory however elegant and economical must be rejected or revised if it is untrue; likewise laws and institutions no matter how efficient and well-arranged must be reformed or abolished if they are unjust. Each person possesses an inviolability founded on justice that even the welfare of society as a whole cannot override."
In the same way, care of the patient is the first virtue of the physician. To a physician, reimbursement, lifestyle, respect, sense of self-worth are all secondary endpoints, and a physician who values these things higher than the patient's care is not a physician at all. The undertaking of medicine necessarily involves sacrifice on the part of the doctor, a setting aside of his own priorities to take on that of the patient, and this is fundamental to the development of trust between the patient and physician that must happen for healing to occur. A patient who does not trust his doctor guts his doctor of the tools of his trade, and a patient cannot trust his doctor unless he knows his doctor prioritizes his care over his own selfish ends.
Furthermore, this ordering of priorities is mandated regardless of who the patient is. The physician must care for and value higher than himself any patient who comes before him; he cannot pick and choose. In the same way that a theory must be dismantled if false or a government must be abolished if unjust, a physician cannot be a physician if he selects who he sees or what he does on the basis of money or insurance.
We are morally obligated to place the patient before ourselves; this is the patient-physician covenant. And as a result, insurance status ought not to influence who we treat. This is an external factor that arises in this ridiculous milieu we call healthcare delivery, and by ridding ourselves of its constraints, we rid ourselves of inadvertently discriminating against the uninsured when this has no bearing on who we treat. We must demand a forum of equality for patients to see doctors; we cannot bar them at the door. This is why healthcare equality - and in this instance, universal insurance - is so important. It allows doctors to do their job, that is, put patients before themselves.
Monday, August 09, 2010
Procedures
As a medical student, procedures are awesome. They're a chance to do something hands-on and daring. We feel like a real doctor, even if it's simply placing an IV or drawing blood. For the most part, procedures are straightforward and safe, even ones that sound intimidating like lumbar puncture or central line. But with a good guiding hand and supervision, it's a great and educational experience.
Interestingly, I've found that as a "real doctor" now, I approach procedures a little differently. I'm the one assessing whether or not the patient needs it, weighing the risks and benefits, and worrying about complications. You might almost imagine a conflict of interest: that because doctors like doing procedures, we might do them unnecessarily. There are certainly cases of this occurring, but I've found that it doesn't happen to me (at least consciously). I try very hard to avoid doing anything risky to my patients, mostly because now they are my patients and it is my job to protect them.
When a procedure comes up, it's also different being a resident. As a medical student, you have someone set everything up and prepare you for success. Now I walk myself through the steps: getting consent, informing the nurses, gathering my supplies, getting the bed into a position that will help me, doing a time out. When you're a student, you skip all of that and go straight into sticking the needle in (or whatever). I've learned that procedures are much more than the act of doing something hands-on; it's the thought that goes into planning it, it's the understanding of the risks and benefits, and it's the anticipation of things that could possibly go wrong.
Interestingly, I've found that as a "real doctor" now, I approach procedures a little differently. I'm the one assessing whether or not the patient needs it, weighing the risks and benefits, and worrying about complications. You might almost imagine a conflict of interest: that because doctors like doing procedures, we might do them unnecessarily. There are certainly cases of this occurring, but I've found that it doesn't happen to me (at least consciously). I try very hard to avoid doing anything risky to my patients, mostly because now they are my patients and it is my job to protect them.
When a procedure comes up, it's also different being a resident. As a medical student, you have someone set everything up and prepare you for success. Now I walk myself through the steps: getting consent, informing the nurses, gathering my supplies, getting the bed into a position that will help me, doing a time out. When you're a student, you skip all of that and go straight into sticking the needle in (or whatever). I've learned that procedures are much more than the act of doing something hands-on; it's the thought that goes into planning it, it's the understanding of the risks and benefits, and it's the anticipation of things that could possibly go wrong.
Sunday, August 08, 2010
Poem: Written While Asleep
This poem was jotted through a half-delirious state.
-
Written While Asleep
all impostors, some time, write an ode to sleep
to sleep, that dog of religion, that half-face
of death, that purveyor of wonder,
that hoard of dream and ferryman return--
sleep, healer in a way I don't understand
that lives in haiku, sung in sonnet,
who hires heroes in times of disbelief
and rocks us sling-swung
over a beak through the air. sleep,
who we strive to behold;
sleep, who owns no possession,
holds us enthralled.
-
Written While Asleep
all impostors, some time, write an ode to sleep
to sleep, that dog of religion, that half-face
of death, that purveyor of wonder,
that hoard of dream and ferryman return--
sleep, healer in a way I don't understand
that lives in haiku, sung in sonnet,
who hires heroes in times of disbelief
and rocks us sling-swung
over a beak through the air. sleep,
who we strive to behold;
sleep, who owns no possession,
holds us enthralled.
Saturday, August 07, 2010
Tablets
 Doctors are traditionally resistant to new technologies, but my generation of physicians include many early adopters. Peek into one of our team rooms and you see smartphones and laptops and perhaps even an iPad sitting around. It'll be really interesting to see what kinds of new innovations will be adopted into the healthcare setting.
Doctors are traditionally resistant to new technologies, but my generation of physicians include many early adopters. Peek into one of our team rooms and you see smartphones and laptops and perhaps even an iPad sitting around. It'll be really interesting to see what kinds of new innovations will be adopted into the healthcare setting.Image is from the Upstream blog, hosted by the Interdisciplinary Health Communication program at the University of North Carolina at Chapel Hill, shown under Fair Use.
Wednesday, August 04, 2010
Life as an Intern
The most important commodity is pens. I carry lots of pens around. I was once amused by a UCSF neurologist whose white coat contained only 10 black pens and a reflex hammer. Now I'm like that.
Friends call me at 9pm. I'm fast asleep.
It's still sort of a novelty that I can sign my notes without a cosignature.
The sound - or even the vibration - of a pager elicits an impending sense of doom and a Pavlovian reflex to touch my hip.
My life revolves around four day cycles rather than seven day weeks. I can never tell you what day of the week it is. I can always tell you when my next call will be.
Food ("GI rounds") is scarce. Well, time is scarce, and food suffers.
The idiosyncrasies of each computer frustrate me. Some have one program but not another. Some crash randomly. Some can't print. When I find a computer that actually works, I hog it.
I've dozed off in the shower. I get home too late to do laundry.
I apologize to friends when I call them retroactively to wish them a happy birthday.
Every week, I expect reminder emails to log my work-hours and fill in my evaluations. I still haven't done them yet.
I usually come home somewhat satisfied, feeling that though I spend way too much time accomplishing what I do each day, at least I am accomplishing something.
Friends call me at 9pm. I'm fast asleep.
It's still sort of a novelty that I can sign my notes without a cosignature.
The sound - or even the vibration - of a pager elicits an impending sense of doom and a Pavlovian reflex to touch my hip.
My life revolves around four day cycles rather than seven day weeks. I can never tell you what day of the week it is. I can always tell you when my next call will be.
Food ("GI rounds") is scarce. Well, time is scarce, and food suffers.
The idiosyncrasies of each computer frustrate me. Some have one program but not another. Some crash randomly. Some can't print. When I find a computer that actually works, I hog it.
I've dozed off in the shower. I get home too late to do laundry.
I apologize to friends when I call them retroactively to wish them a happy birthday.
Every week, I expect reminder emails to log my work-hours and fill in my evaluations. I still haven't done them yet.
I usually come home somewhat satisfied, feeling that though I spend way too much time accomplishing what I do each day, at least I am accomplishing something.
Tuesday, August 03, 2010
Learning on the Job
UCSF trained me well. I find that I actually know most of the medical facts I need on a day-to-day basis. Although of course I'm constantly reviewing and relearning things, I was surprised to realize internship is less about rounding out my fund of knowledge and more about learning to apply it. The application, though, is a whole different story. As medical students, we learn to anticipate pimping, getting asked questions by an attending. We learn to review Calot's triangle before scrubbing into a cholecystectomy; that if we're placing an arterial line, we'll get asked about the Allen test; or if a patient has an EKG, we'll be asked to read it. And we get pretty good at answering these questions.
But now as a resident, I don't have the luxury of having my questions be hypothetical. When I am forced to think about fever, it's not to answer a question from an attending, it's because my patient's temperature is high. When a nurse calls to tell me my patient's blood pressure is 200/40, I need to figure out why. That transition from simply answering a question on rounds to committing to a clinical judgment for a patient is everything about being a resident.
I've been faced with half a dozen clinical situations where there's a vast chasm between knowing the right answer and committing to it. On my second night on call in the ICU, a patient developed acute atrial fibrillation, a problem whose UpToDate article I've read half a dozen times. But the difference between answering amiodarone to an attending's question and writing out that bolus and drip is remarkable. I second guess myself all the time. Is this right? How sure am I? The stakes are so much higher; as a medical student, we risk our grades when we take a stab at an answer; as a resident, we're responsible for someone's well-being.
My third night on call, I had to manage a vasopressor in a patient who was hypotensive. He was dialysis-dependent with end stage renal disease, and that meant I had to balance giving fluids with titrating my drugs. I spent most of the night at the bedside, evaluating, re-evaluating, adjusting up, adjusting down, and it taught me that there is no substitute for experience. I had read the textbook chapter on vasopressors, but I never fully understood them until I spent an entire night awake keeping this patient alive. The growth curve and transition from student to resident is actually quite remarkable, and I've been thinking about it a lot lately.
But now as a resident, I don't have the luxury of having my questions be hypothetical. When I am forced to think about fever, it's not to answer a question from an attending, it's because my patient's temperature is high. When a nurse calls to tell me my patient's blood pressure is 200/40, I need to figure out why. That transition from simply answering a question on rounds to committing to a clinical judgment for a patient is everything about being a resident.
I've been faced with half a dozen clinical situations where there's a vast chasm between knowing the right answer and committing to it. On my second night on call in the ICU, a patient developed acute atrial fibrillation, a problem whose UpToDate article I've read half a dozen times. But the difference between answering amiodarone to an attending's question and writing out that bolus and drip is remarkable. I second guess myself all the time. Is this right? How sure am I? The stakes are so much higher; as a medical student, we risk our grades when we take a stab at an answer; as a resident, we're responsible for someone's well-being.
My third night on call, I had to manage a vasopressor in a patient who was hypotensive. He was dialysis-dependent with end stage renal disease, and that meant I had to balance giving fluids with titrating my drugs. I spent most of the night at the bedside, evaluating, re-evaluating, adjusting up, adjusting down, and it taught me that there is no substitute for experience. I had read the textbook chapter on vasopressors, but I never fully understood them until I spent an entire night awake keeping this patient alive. The growth curve and transition from student to resident is actually quite remarkable, and I've been thinking about it a lot lately.
Monday, August 02, 2010
Poem: Departure
Departure
I would like to see you
I would like to see you through
I would like
to see you float, how you wisp
how you raven-bound blow
from olive tree to oak
how you buoy up
tide’s depth unrelentless
secret-whisper a notebook
you hide in your dresser
lists of lovers by lovers
would like to see
you dance, hoisted overhead
chairs dangling, to see you work
sanding, sawing, see you stretch
down to earth, see you sing
hearth and heartland. I would like
you to sing again
would like you to sing
to my trodden head
to sing sleep a sound
song a lullabye.
I would like you to hum
as I fall asleep.
I would like to see you
I would like to see you through
I would like
to see you float, how you wisp
how you raven-bound blow
from olive tree to oak
how you buoy up
tide’s depth unrelentless
secret-whisper a notebook
you hide in your dresser
lists of lovers by lovers
would like to see
you dance, hoisted overhead
chairs dangling, to see you work
sanding, sawing, see you stretch
down to earth, see you sing
hearth and heartland. I would like
you to sing again
would like you to sing
to my trodden head
to sing sleep a sound
song a lullabye.
I would like you to hum
as I fall asleep.
Subscribe to:
Posts (Atom)


