Sunday, November 30, 2014
Thanksgiving in the Hospital
I've always wanted to know how holidays compare to a regular day in the hospital. In the intensive care unit, I don't know that there's a huge difference. Although we have no scheduled surgeries requiring post-operative ICU care, we do see an uptick in the wayward patient who overindulges. For example, when I was on my 24-hour Thanksgiving shift, I saw a couple patients who had a little too much salt. Although one avoided the ICU, the other had to come up for dialysis to take off that extra turkey brine and wine. I have a suspicion that the days after a major holiday might see an uptick in admissions with all those who were sick on Thanksgiving but didn't want to come in owing to the holiday. When I get back to work tomorrow, I'll find out. I hope your Thanksgiving was healthy, happy, and away from the hospital.
Wednesday, November 26, 2014
Thanksgiving
This year, I am thankful to be finally reaching the end of my training. It has been an awfully long road, so long that the sacrifices seem normal. I can't remember the last time I flew home to my parents' for Thanksgiving. That doesn't bother me per se, but rather the thought that my parents have missed out on me being home for the last eight years or so. Holiday after holiday, weekend after weekend, the hospital has become a second home, my co-residents a second family. All this changes in a little over six months, and I'm not sure how I'll take it. I've adapted to this lifestyle, and really, I love it. I enjoy the role I have in the hospital, the gradated learning, the work I do. It's immensely fulfilling and at the same time immensely tiring. I hope that when I finish fellowship, I'll find a career that offers me the same deeply satisfying work for a little better compensation and work-life balance. For that, this year, though I will be in the intensive care unit all day and all night, I am grateful.
Sunday, November 23, 2014
Social Media
For a long time, I didn't bother much with social media. Although I think social media is exciting and has the potential to be influential, I tend to be a late adopter of technologies. I never craved garnering lots of followers or developing a social media reputation. However, over the last few years, I've slowly developed more of an online presence, and I like it. I've always tried to put good content up, and though I don't have flashy videos, graphics, or designs, I hope that some of my thoughts on medicine are worth readings.
Recently, several of my blogs for The American Resident Project have been picked up by KevinMD. Most recently, I wrote a commentary on quality ratings for health care providers in the U.S. A list of all the posts he's reblogged can be found here. I think cross-pollination is important because solving health care problems is a discussion, and I want to engage others (like you!) in conversation. I do appreciate it if you follow this blog, rebroadcast ideas, and leave comments. My goal isn't popularity or number of hits, but focusing attention on medical stories, problems, and ideas so we can improve health care as a whole. Thank you for those you already read, follow, or comment. It helps me justify those late nights researching and writing these blogs.
Recently, several of my blogs for The American Resident Project have been picked up by KevinMD. Most recently, I wrote a commentary on quality ratings for health care providers in the U.S. A list of all the posts he's reblogged can be found here. I think cross-pollination is important because solving health care problems is a discussion, and I want to engage others (like you!) in conversation. I do appreciate it if you follow this blog, rebroadcast ideas, and leave comments. My goal isn't popularity or number of hits, but focusing attention on medical stories, problems, and ideas so we can improve health care as a whole. Thank you for those you already read, follow, or comment. It helps me justify those late nights researching and writing these blogs.
Thursday, November 20, 2014
Book Review: God's Hotel
I got several recommendations to read Victoria Sweet's nonfiction book, God's Hotel. An anesthesiologist who does creative writing and a resident in internal medicine both recently read this book and told me about it. When I looked at the jacket description, I knew why. Victoria Sweet explores the fascinating history and modern reimagination of one of the oldest institutions in San Francisco, Laguna Honda Hospital. For Bay Area physicians, it's especially personal because we've often sent patients to and received patients from Laguna Honda. Initially an almshouse, Laguna Honda inherited the role of caring for the poor and indigent of San Francisco, those who have nowhere else to go. It plays a critical role in the health care safety net of the city, a place for rehabilitation, AIDS patients, dementia, and chronic illness. Victoria Sweet paints a vivid picture of its history and occupants and describes its rocky recent history as budget cuts, increased regulations, and political powerplays threaten its existence. This, too, is relevant to me because when I was a medical student, I heard a lot about the various propositions regarding Laguna Honda. I drove past it regularly, but never investigated its character - its beautiful landscape, historic architecture, and unusual throwbacks to the past.
Along with describing the history of an institution, Victoria Sweet writes about her growth as a physician, interesting patient cases, and opinions on modern medicine. As a blogger who enjoys writing clinical vignettes, I liked reading her patient encounters, fun diagnoses, and descriptions of complex medical phenomena; she does a great job making it accessible to the lay public. I also agree a lot with her commentary on what's important in medicine. Although the book does not primarily seek to change the way medicine is practiced, she makes a case for returning medicine to its roots. She describes the growth of bureaucracy, regulation of medicine, influence of lawsuits, and tightening budgets affecting health care. I was shocked to learn how much administrators, politicians, and bureaucrats interfere with the delivery of medicine at Laguna Honda. I got a glimpse into the community, charity, and values of medicine of a by-gone era.
Lastly, Victoria Sweet weaves in her own personal interest, a journey into understanding medieval history of medicine. She describes tenants of pre-modern medicine such as how to treat the evil humors. She writes about her studies, sabbaticals, and pilgrimages to understand history of medicine. Though this was least interesting to me, it gave me appreciation of the many facets of our profession. Overall, God's Hotel was an enjoyable nonfiction book with a lot of relevance for a Bay Area doctor. Of the many books out there written by physicians, I thought this was one of the more unique and worthwhile.
Image from victoriasweet.com, shown under Fair Use.
Tuesday, November 18, 2014
Ondine's Curse and Other Unusual Causes for Respiratory Failure
There's a short list of really common reasons patients may need a mechanical ventilator in the intensive care unit: pneumonia, acute respiratory distress syndrome, pulmonary edema, hypercarbic respiratory failure, altered mental status. But at a tertiary referral center like Stanford, we get a few rare causes of respiratory failure. A few months ago, I admitted a patient who was simply too weak to take a deep breath. She was young, but she had a rhematologic illness that infiltrated her central (proximal) muscles. She went from working full time to being completely bedbound and gasping for air within months. After confirming the diagnosis with nerve and muscle conduction studies and a muscle biopsy, we started high dose immunosuppressants. Soon she was walking around the ICU on a ventilator. With good rehabilitation and rheumatologic followup, we hope that she will regain the ability to breathe.
Another patient has a more unfortunate disease. She has a tumor in her brainstem right at the center that controls subconscious breathing. This is a big problem; she is effectively cursed by Ondine. Ondine was a water nymph who had a unfaithful mortal lover, so she cursed him so that if he fell asleep, he would stop breathing (he had previously vowed that every waking breath was a testimony of his love). This patient suffered two cardiac arrests from apnea - she stopped breathing, and there was no automatic stimulus or drive to breathe. Normally, our brainstem regulates our breathing pattern while we are asleep, but the location of her brain tumor disrupts those signals. During the daytime, she is fine, but when she falls asleep, she needs a backup rate to breathe for her through a tracheostomy. She, too, will do fine; her brain cancer is benign, but she will need to be in a long term ventilator facility, and we need to see if chemotherapy and steroids shrink the tumor such that she remembers to breathe again.
First image of a mechanical ventilator shown under Creative Commons Attribution Share-Alike License, from Wikipedia. Second image of John William Waterhouse's painting of Ondine is in the public domain, from Wikipedia.
Sunday, November 16, 2014
First, Do No Harm
Pre-liver transplant patients have a unique clinical situation. Their cirrhosis is irreversible; the only way to treat the underlying cause of their problems is a liver transplant. But unlike other therapies, transplants are unpredictable; a "patient" (pun not intended) might have to wait two days or a month to get their transplant. Even worse, they may have a complication that takes them off the transplant list before they can get an organ. In our hospital, we have far more patients than organs so that those who get the organ have been waiting a long time, and consequently, have far more advanced disease.
Liver disease invites complications. If the liver cannot clear the evil humours in the blood, patients get confused which begets more complications. Cirrhosis decouples blood pressure regulatory mechanisms, it invites pulmonary arterio-venous malformation development, it changes pressures in the brain. The gastrointestinal system becomes engorged with blood, leading to risk for bleeding. The liver stops producing proteins and platelets that stop bleeding. If the liver's synthesis of anti-infectious agents wanes, then infectious become more common and more deadly. The liver's function is intricately tied to the kidney, and when the liver starts failing, the kidney is at risk to do so as well.
We see all these complications in our pre-transplant patients, and as their disease progresses, they come up to the ICU. They come because their confusion requires intubation, their infections require brood spectrum antibiotics, their gastrointestinal bleeds require massive transfusions, their kidneys require continuous dialysis, their blood pressures require continuous vasopressor support. But the most important thing for us to remember is for these patients especially, first do no harm. Our ultimate goal is to get them the transplant, so we have to be cognizant of every risk the patient is exposed to. If we place a central line that gets infected, if we give antibiotics that lead to a Clostridium dificile infection, if we fail to protect their kidneys, if we don't give adequate nutrition, they may lose their place on the transplant list. In contrast to the other patients in the ICU whose diseases we can reverse and who we can get better, we only hope to keep our pre-transplant patients where they are so they can get an organ.
It does work and amazingly so. A woman with alcoholic cirrhosis was on my ICU service three weeks getting daily transfusions and continuous dialysis. After waiting day after day, she finally got a liver. She was walking the second day after surgery and left the ICU four days after her transplant. We expect her kidneys to get better. She has a new life.
Both images are in the public domain, from Wikipedia. First image is a healthy liver. Second image shows cirrhosis.
We see all these complications in our pre-transplant patients, and as their disease progresses, they come up to the ICU. They come because their confusion requires intubation, their infections require brood spectrum antibiotics, their gastrointestinal bleeds require massive transfusions, their kidneys require continuous dialysis, their blood pressures require continuous vasopressor support. But the most important thing for us to remember is for these patients especially, first do no harm. Our ultimate goal is to get them the transplant, so we have to be cognizant of every risk the patient is exposed to. If we place a central line that gets infected, if we give antibiotics that lead to a Clostridium dificile infection, if we fail to protect their kidneys, if we don't give adequate nutrition, they may lose their place on the transplant list. In contrast to the other patients in the ICU whose diseases we can reverse and who we can get better, we only hope to keep our pre-transplant patients where they are so they can get an organ.
It does work and amazingly so. A woman with alcoholic cirrhosis was on my ICU service three weeks getting daily transfusions and continuous dialysis. After waiting day after day, she finally got a liver. She was walking the second day after surgery and left the ICU four days after her transplant. We expect her kidneys to get better. She has a new life.
Both images are in the public domain, from Wikipedia. First image is a healthy liver. Second image shows cirrhosis.
Friday, November 14, 2014
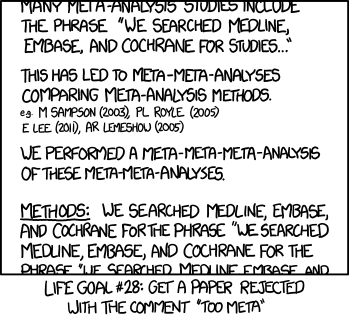
Meta-analysis
Often considered the "best" type of studies, meta-analyses compile data from smaller, more primary studies to generate more powerful conclusions. It's like doing research on previous research. But how meta can you get?
Image is from xkcd, drawn by Randall Munroe, shown under Creative Commons Attribution License.
Image is from xkcd, drawn by Randall Munroe, shown under Creative Commons Attribution License.
Tuesday, November 11, 2014
Grief and Loss
One of my friends from high school recently lost her husband to cancer. Watching her go through this ordeal really struck home to me that visceral feeling of grief and loss. Working in intensive care, we see so many families in distress with the illness or loss of a family member. I try to remain cognizant of these emotions and hope that I express enough empathy for these families. But it's really something different when it's someone you know, someone your age, someone whose shoes you really could have worn.
It is a terrible process, long, agonizing, fighting uphill every step of the way. I watched her struggle with insurance denials, second opinions, discouraging MRI and PET scan results, unexpected hospitalizations, and the struggle to transition to hospice. From a intellectual, medical standpoint, I understood everything; I've seen the process so many times. But it was pain and heartache, grief and loss hearing my friend go through this.
My thoughts go to all those struggling with medical illness and all those caretakers who put their whole heart into it and still come out heartbroken.
It is a terrible process, long, agonizing, fighting uphill every step of the way. I watched her struggle with insurance denials, second opinions, discouraging MRI and PET scan results, unexpected hospitalizations, and the struggle to transition to hospice. From a intellectual, medical standpoint, I understood everything; I've seen the process so many times. But it was pain and heartache, grief and loss hearing my friend go through this.
My thoughts go to all those struggling with medical illness and all those caretakers who put their whole heart into it and still come out heartbroken.
Saturday, November 08, 2014
Teaching and Doing Procedures in the ICU
Placement of a central venous catheter is a core skill on most medical specialties. Emergency physicians, surgeons, internal medicine doctors, anesthesiologists, and pediatricians all have to learn to place a "central line." In principle, it's easy: place a needle into a central vein, thread a wire through that needle, and place a catheter over that wire. But in practice, there's a learning curve, and as an ICU fellow, I have to shepherd residents through that learning curve by supervising their procedures.
This has taught me a lot. I've learned where obstacles seem to crop up for trainees. Some are simply nuisances, inefficiencies, but some can be potentially harmful. I quickly learn to recognize how comfortable a medical student or resident is in the process; some just need a nod of reassurance, and some need me to scrub and hold their hand; some don't recognize how little they know, and some don't recognize how skilled they actually are. I spend a lot of time thinking of how to best teach a particular trainee; inundate a newbie with too much information and they will be overwhelmed, but even a proficient proceduralist (including myself) has things to learn. For example, if someone has done a hundred lines, I still find things to teach. How do you do the line completely solo with no assistance? (How do you adjust the ultrasound knobs or place the probe cover when you're already sterile?) How can you maximize efficiency? How can you do the line without a drop of blood touching the patient's bed? My background as an anesthesiologist really helps me in this setting; I've had my share of pressure for efficiency in the OR and learned many tricks from placing regional nerve blocks.
The learning curve is steep at first and then plateaus. After doing a couple dozen lines, most physicians can handle straightforward central lines with ease. However, we occasionally have very high risk clinical situations, and that's when for patient safety, I do the lines myself. Trauma, obesity, prior lines and surgeries, altered anatomy, inability to tolerate usual positioning are all reasons a central line can be scary, but my most challenging line (and the one I'm most proud of) was for a dying liver patient.
The patient, who already had multiple neck central lines, needed emergent dialysis. He was extremely prone to bleeding from disseminated intravascular coagulation with an INR of 6. Cognizant of following my own advice, I set everything up carefully. Once I started, I had to move quickly because bleeding would start immediately, and a hematoma might make the procedure impossible. The patient's abdominal ascites from cirrhosis made femoral access difficult, but it was the best vein I had. With one quick stab into the femoral vein, the patient started oozing blood, even with a small 18 gauge finder needle (1.3mm diameter). With two quick dilations, I managed to slip the 12.5 French (4.2mm diameter) trialysis catheter into place. I was pretty sweaty as I did it. I am no surgeon, but sometimes I like that feeling when a challenge is presented and I use all my skills and experience to conquer it.
Image is in the public domain.
This has taught me a lot. I've learned where obstacles seem to crop up for trainees. Some are simply nuisances, inefficiencies, but some can be potentially harmful. I quickly learn to recognize how comfortable a medical student or resident is in the process; some just need a nod of reassurance, and some need me to scrub and hold their hand; some don't recognize how little they know, and some don't recognize how skilled they actually are. I spend a lot of time thinking of how to best teach a particular trainee; inundate a newbie with too much information and they will be overwhelmed, but even a proficient proceduralist (including myself) has things to learn. For example, if someone has done a hundred lines, I still find things to teach. How do you do the line completely solo with no assistance? (How do you adjust the ultrasound knobs or place the probe cover when you're already sterile?) How can you maximize efficiency? How can you do the line without a drop of blood touching the patient's bed? My background as an anesthesiologist really helps me in this setting; I've had my share of pressure for efficiency in the OR and learned many tricks from placing regional nerve blocks.
The learning curve is steep at first and then plateaus. After doing a couple dozen lines, most physicians can handle straightforward central lines with ease. However, we occasionally have very high risk clinical situations, and that's when for patient safety, I do the lines myself. Trauma, obesity, prior lines and surgeries, altered anatomy, inability to tolerate usual positioning are all reasons a central line can be scary, but my most challenging line (and the one I'm most proud of) was for a dying liver patient.
The patient, who already had multiple neck central lines, needed emergent dialysis. He was extremely prone to bleeding from disseminated intravascular coagulation with an INR of 6. Cognizant of following my own advice, I set everything up carefully. Once I started, I had to move quickly because bleeding would start immediately, and a hematoma might make the procedure impossible. The patient's abdominal ascites from cirrhosis made femoral access difficult, but it was the best vein I had. With one quick stab into the femoral vein, the patient started oozing blood, even with a small 18 gauge finder needle (1.3mm diameter). With two quick dilations, I managed to slip the 12.5 French (4.2mm diameter) trialysis catheter into place. I was pretty sweaty as I did it. I am no surgeon, but sometimes I like that feeling when a challenge is presented and I use all my skills and experience to conquer it.
Image is in the public domain.
Thursday, November 06, 2014
Families
One of the harder responsibilities as an ICU fellow is dealing with the frustrated, disgruntled, upset, or angry patient or family member. Fortunately, we don't encounter this too often, but it does happen, and those conversations and interactions are really tough. I really believe that emotions like these are understandable; I've never been hospitalized in the ICU or had a direct family member in that situation, but I can imagine how hard it must be. There is always room for more empathy, better communication, fewer complications, and improved support in the ICU. I think that most people who are upset are learning to cope with having a loved one in a critically ill condition.
I write this blog, though, to describe how challenging it is to be in this situation. Although sometimes, we get advance notice from a nurse that a family member is angry, we are often blindsided in this situations. Grievances sometimes involve things that I (or my team) was not involved in such as missed diagnoses at an outside hospital, delays in the emergency department, or the cost of parking. However, there are aspects of ICU medicine for which we are guilty such as poor communication with the family. I often view my role in these family meetings as explaining the clinical situation and allowing family members to vent. In the last few months, I've learned a lot about handling these situations. A quiet room, a calm demeanor, open ended questions, acknowledge a family member's sentiments, and when arguing will just get you into trouble all go a long way to improving relationships with families.
I write this blog, though, to describe how challenging it is to be in this situation. Although sometimes, we get advance notice from a nurse that a family member is angry, we are often blindsided in this situations. Grievances sometimes involve things that I (or my team) was not involved in such as missed diagnoses at an outside hospital, delays in the emergency department, or the cost of parking. However, there are aspects of ICU medicine for which we are guilty such as poor communication with the family. I often view my role in these family meetings as explaining the clinical situation and allowing family members to vent. In the last few months, I've learned a lot about handling these situations. A quiet room, a calm demeanor, open ended questions, acknowledge a family member's sentiments, and when arguing will just get you into trouble all go a long way to improving relationships with families.
Tuesday, November 04, 2014
Ebola VI - What It Means for Me
As a critical care fellow, I'm likely to be one of the physicians taking care of patients with suspected or proven Ebola. It's a fascinating and crazy process. One of our first training sessions involved learning to put on and take off our personal protective equipment. It's a real process; the guide has 38 steps for donning the equipment and 27 steps for doffing it (which, by the way, is now one of my favorite words). We wear helmets with built-in fans normally sported by orthopedic surgeons to ventilate our suits while we work. We have three pairs of gloves, three layers of footwear. Walking feels strange, and placing an IV is a challenge. With three layers of gloves, I can barely palpate veins. Our body is protected by an impermeable suit and impervious surgical gown. I spent half an hour in the get-up, practicing intubating mannequins, placing IVs, and manipulating equipment, and by the end, under all those layers, I had worked up a sweat.
The real danger is taking off the equipment because that's when things are contaminated. There is a strict protocol and order in which everything is done including when we step out of the patient's room to the antechamber and when we're allowed to leave the antechamber. Currently, the way things are set up, there will always be a health care practitioner in the room, one in the antechamber to help, and two outside the room as well as a safety officer overseeing compliance with all of this.
Even though the diagnosis and treatment of Ebola virus disease is not necessarily complicated, as we plan for this potential threat, I'm learning how even for a relatively straightforward disease, we will have to implement new and complex protocols for physicians and other health care workers.
Image of an air-transportable isolation module is in the public domain, from Wikipedia.
Sunday, November 02, 2014
Ebola V - What It Means for U.S. Hospitals
In the past few blogs, I've talked about Ebola in West Africa. Nevertheless, most of us aren't going to West Africa, even if we recognize how important that is. For the less daring, less courageous of us, we focus on preparations at home. Now that there are several cases of Ebola in the U.S., it is no longer a possibility or threat; it's real. Fortunately, we have the resources here to take care of it. What does this look like? What does this mean?
I've been privy to some of the discussions and preparations at Stanford Hospital for managing new and emerging infectious diseases like Ebola. It is a process that involves a lot of people and departments. The physicians likely to encounter Ebola are emergency doctors, infectious disease specialists, and critical care physicians. But those at greatest risk will be those who have the most contact with Ebola patients, our nurses. We also have to involve administration, facilities management (how do you dispose of all the Ebola-contaminated gowns?), respiratory therapy, and the county public health office. We have to figure out our processes and policies. For example, what do you do if a potential Ebola patient has a cardiac arrest? If health care workers swarm into the room, they are likely to get exposed, even if they try to put on personal protective equipment. Do we send these patients to the MRI or CT scanner? How do we prevent potential infected persons from sitting in a waiting room? And though we all expect patients to enter the health care system through the emergency department or urgent care, it's entirely possible that they can show up to an unrelated clinic or satellite center.
Although these decisions are still undergoing review, we're using technology to our advantage. For example, to limit the health care workers directly in contact with a patient, we're considering putting cameras in patient rooms so physicians can talk to patients without going into the room. That way, specialists like infectious disease doctors can do most of their job without endangering themselves. We're coming up with the exact route a patient will take from the emergency department to the ICU room and how security will facilitate that transport. We're determining the appropriate number of nurses, the length of nursing shifts, and the appropriate level of evaluation - for example, with the biohazard suits, we cannot listen to the heart or lungs with a stethoscope. We have gotten chemicals that solidify waste to make it more manageable. Our office of emergency response and disasters has already put dozens of health care workers through the training for putting on the biohazard equipment.
Image of researcher in biosafety level 4 hazmat suit is in the public domain, from Wikipedia.
I've been privy to some of the discussions and preparations at Stanford Hospital for managing new and emerging infectious diseases like Ebola. It is a process that involves a lot of people and departments. The physicians likely to encounter Ebola are emergency doctors, infectious disease specialists, and critical care physicians. But those at greatest risk will be those who have the most contact with Ebola patients, our nurses. We also have to involve administration, facilities management (how do you dispose of all the Ebola-contaminated gowns?), respiratory therapy, and the county public health office. We have to figure out our processes and policies. For example, what do you do if a potential Ebola patient has a cardiac arrest? If health care workers swarm into the room, they are likely to get exposed, even if they try to put on personal protective equipment. Do we send these patients to the MRI or CT scanner? How do we prevent potential infected persons from sitting in a waiting room? And though we all expect patients to enter the health care system through the emergency department or urgent care, it's entirely possible that they can show up to an unrelated clinic or satellite center.
Although these decisions are still undergoing review, we're using technology to our advantage. For example, to limit the health care workers directly in contact with a patient, we're considering putting cameras in patient rooms so physicians can talk to patients without going into the room. That way, specialists like infectious disease doctors can do most of their job without endangering themselves. We're coming up with the exact route a patient will take from the emergency department to the ICU room and how security will facilitate that transport. We're determining the appropriate number of nurses, the length of nursing shifts, and the appropriate level of evaluation - for example, with the biohazard suits, we cannot listen to the heart or lungs with a stethoscope. We have gotten chemicals that solidify waste to make it more manageable. Our office of emergency response and disasters has already put dozens of health care workers through the training for putting on the biohazard equipment.
Image of researcher in biosafety level 4 hazmat suit is in the public domain, from Wikipedia.
Subscribe to:
Posts (Atom)






.jpg)



