How can we lower the barriers to counseling? Like medical or dental insurance, I think mental health and personal well-being resources should be available to anyone. Depression, grief, anger, and addiction can be just as life-altering as cavities or a broken bone or a heart attack. No one should have to pay hundreds of dollars out of pocket to address these issues. And I think ultimately, society will benefit. With good counseling, patients may need fewer medications, be more productive, and be less likely to get involved with gangs, drugs, and violence. We need to increase the number of providers, lower the cost of getting help, and expand access to this critical resource.
Sunday, July 31, 2016
Therapy and Socioeconomic Status
One thing about therapy and counseling that troubles me is the cost. I've always been surprised by how expensive it can be, and not all therapists accept insurance. What they do is amazing and certainly worth the price, but the expense means there are be barriers to access. Mental illness is certainly more prevalent in populations that are poorer, though this is correlative and not causative. But even aside from psychiatric disease, many people simply need counseling for itself; we go through hurt, loss, and tragedy, and most of us don't have extraordinary coping skills.
Thursday, July 28, 2016
CRISPR
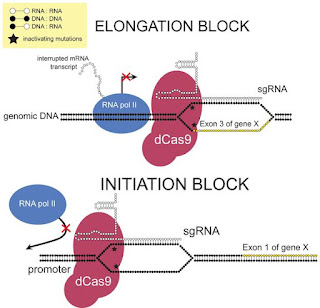
To be honest, I haven't looked at the scientific papers behind CRISPR, but I've read a lot of lay articles about this genomic editing technique. As I understand, CRISPR stands for clustered regularly interspaced short palindromic repeats and represents sections of DNA that confers resistance to foreign genetic elements. They are found in bacteria and act as a way to recognize and cut out foreign DNA sequences.
The applications of this system are staggering. By using CRISPR and associated genes (called Cas), scientists are able to precisely and easily manipulate the genetics of most cells, including human ones. The technology has been used to knock out specific genes and add specific genetic sequences. Genes can be turned on or off in almost any organism. Most importantly, though, this technology is easy to use and effective.
Various laboratories around the world are using CRISPR/Cas to create disease-resistant crops, mosquitoes that won't spread malaria, yeasts that make biofuels, and animal models of various diseases. The beneficial implications are profound; we really might be entering an age where genetic modification is widespread. But the dangers are clear; such technologies can be used for evil; bioterrorists could conceivably create diseases that are much more virulent and deadly.
One of the most debated controversies, however, is the genetic editing of germline cells. The technology can be used to change the genomes of sperm, eggs, and embryos, and such changes would be permanent and passed onto offspring. This is really close to "playing God." The changes that we make might have dramatic unforeseen consequences. Without close scientific scrutiny, research, and forethought, embryo engineers may cause irrevocable damage to the human genome. We don't yet understand how all our genes interact, and we wouldn't know the implications of altering one gene, even if we did so with admirable intent.
In addition, the ability to have "designer babies" is ethically fraught. If we edit the genome to eliminate sickle cell disease, for example, what does that say about living people with sickle cell? It becomes a slippery slope to social Darwinism and eugenics by saying certain types of people should not exist. What if unethical genetic engineers moved from diseases to other traits like height or intelligence? Such possibilities are really not that far off; the dangers of unregulated genetic editing of embryos really worry me.
I don't pay that much attention to basic science breakthroughs these days; although I would love to stay current with such things, it just doesn't apply to my day-to-day life. Discoveries like this, however, catch my attention because of the widespread scientific, medical, cultural, social, and ethical implications. The ability to engineer genomes is a potential gamechanger in medical research, agriculture, biology (some scientists are considering reviving extinct species), bioengineering, and a dozen other applications. But it can be ethically fraught if we start playing God and exerting our own will on the forces of evolution.
Image shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
The applications of this system are staggering. By using CRISPR and associated genes (called Cas), scientists are able to precisely and easily manipulate the genetics of most cells, including human ones. The technology has been used to knock out specific genes and add specific genetic sequences. Genes can be turned on or off in almost any organism. Most importantly, though, this technology is easy to use and effective.
Various laboratories around the world are using CRISPR/Cas to create disease-resistant crops, mosquitoes that won't spread malaria, yeasts that make biofuels, and animal models of various diseases. The beneficial implications are profound; we really might be entering an age where genetic modification is widespread. But the dangers are clear; such technologies can be used for evil; bioterrorists could conceivably create diseases that are much more virulent and deadly.
One of the most debated controversies, however, is the genetic editing of germline cells. The technology can be used to change the genomes of sperm, eggs, and embryos, and such changes would be permanent and passed onto offspring. This is really close to "playing God." The changes that we make might have dramatic unforeseen consequences. Without close scientific scrutiny, research, and forethought, embryo engineers may cause irrevocable damage to the human genome. We don't yet understand how all our genes interact, and we wouldn't know the implications of altering one gene, even if we did so with admirable intent.
In addition, the ability to have "designer babies" is ethically fraught. If we edit the genome to eliminate sickle cell disease, for example, what does that say about living people with sickle cell? It becomes a slippery slope to social Darwinism and eugenics by saying certain types of people should not exist. What if unethical genetic engineers moved from diseases to other traits like height or intelligence? Such possibilities are really not that far off; the dangers of unregulated genetic editing of embryos really worry me.
I don't pay that much attention to basic science breakthroughs these days; although I would love to stay current with such things, it just doesn't apply to my day-to-day life. Discoveries like this, however, catch my attention because of the widespread scientific, medical, cultural, social, and ethical implications. The ability to engineer genomes is a potential gamechanger in medical research, agriculture, biology (some scientists are considering reviving extinct species), bioengineering, and a dozen other applications. But it can be ethically fraught if we start playing God and exerting our own will on the forces of evolution.
Image shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Monday, July 25, 2016
Self-Fulfilling Prophecies
Doctors are a strange bunch. We champion science and evidence based medicine, quoting the latest research journal or study. But we are also a little superstitious, though we don't like to admit it. We talk about our "clouds" - whether we attract business or not when we are on call. I once had a resident who, taunting our superstitious natures, would declare on call, "Not even God can sink this ship." Without fail, those nights exhausted us with endless admissions.
I was telling this story to another physician, and when I started it, she said, "I bet the patient had a C-section." The story starts like this. A woman walks into labor and delivery closely followed by her doula, birthing ball, and yoga mat. She has a typed five page document with her birth plan, a smooth satisfying natural child birth.
Although some physicians roll their eyes, I support mothers like this. In my first year of medical school, I took an elective to see the childbirth process from a patient's point of view, and I trained in one of the most hippie-friendly open-minded areas of the country. I champion patient decision making. Complementary and alternatives approaches to medicine intrigue me.
But alas, the superstitious of us might believe that she sealed her fate with a self-fulfilling prophecy. Over the next few days, she needed induction with escalating doses of oxytocin and became more and more exhausted when the process of labor dragged out. Finally, after several days without sleep, she decided to get an epidural. By now, the idealistic and lofty goals of the perfect delivery were out the door. She struggled with her pre-formulated plan, asking the obstetrician whether she should get a Cesarean (which, on a totally separate note, would be a great spelling bee word; I never get it right).
Of course, she ended up going to C-section for arrest of descent, and of course it was at three in the morning. Because of her prolonged labor, her uterus would not contract after delivery and she had massive bleeding. We activated the massive transfusion protocol. Of course, her IV access was poor and I was under the drapes putting in extra IVs so she could get fluids and blood. She required everything we could think of: oxytocin, methylergonovine, prostaglandins, misoprostol, a Bakri balloon. We almost called interventional radiology.
Fortunately, she had a healthy baby and her anesthesia was well maintained with her epidural. She never needed to go to the intensive care unit and got through the whole ordeal just requiring a few units of blood. We go through our lives trying to plan as much as we can, certain we know what would make us happiest. But the superstitious among us know that sometimes when that patient with a doula and birth document comes in, it might be prudent to plan for the worst.
I was telling this story to another physician, and when I started it, she said, "I bet the patient had a C-section." The story starts like this. A woman walks into labor and delivery closely followed by her doula, birthing ball, and yoga mat. She has a typed five page document with her birth plan, a smooth satisfying natural child birth.
Although some physicians roll their eyes, I support mothers like this. In my first year of medical school, I took an elective to see the childbirth process from a patient's point of view, and I trained in one of the most hippie-friendly open-minded areas of the country. I champion patient decision making. Complementary and alternatives approaches to medicine intrigue me.
But alas, the superstitious of us might believe that she sealed her fate with a self-fulfilling prophecy. Over the next few days, she needed induction with escalating doses of oxytocin and became more and more exhausted when the process of labor dragged out. Finally, after several days without sleep, she decided to get an epidural. By now, the idealistic and lofty goals of the perfect delivery were out the door. She struggled with her pre-formulated plan, asking the obstetrician whether she should get a Cesarean (which, on a totally separate note, would be a great spelling bee word; I never get it right).
Of course, she ended up going to C-section for arrest of descent, and of course it was at three in the morning. Because of her prolonged labor, her uterus would not contract after delivery and she had massive bleeding. We activated the massive transfusion protocol. Of course, her IV access was poor and I was under the drapes putting in extra IVs so she could get fluids and blood. She required everything we could think of: oxytocin, methylergonovine, prostaglandins, misoprostol, a Bakri balloon. We almost called interventional radiology.
Fortunately, she had a healthy baby and her anesthesia was well maintained with her epidural. She never needed to go to the intensive care unit and got through the whole ordeal just requiring a few units of blood. We go through our lives trying to plan as much as we can, certain we know what would make us happiest. But the superstitious among us know that sometimes when that patient with a doula and birth document comes in, it might be prudent to plan for the worst.
Monday, July 18, 2016
Studying This Week
Hello, and thank you for reading my blog. I am gearing up for my (hopefully final) set of board examinations (for about a decade at least). Critical care medicine boards are in less than a month so I'm going to take this week off from blogging to focus on reading. I'll be back in a week.
Craig
Craig
Friday, July 15, 2016
Separation and Globalization
The "Brexit" movement is fascinating to me because of some parallels with the medical world. Those who voted for Britain to leave the European Union were mostly older (59% of those 65+ voted to leave compared to 19% of those 18-24), who experienced England before the E.U., who were hurt by globalization. I don't pretend to understand the complex political milieu, but I sense parallels in medicine. There is a globalization of medicine that has been occurring and will continue to change the way we practice. Several generations ago, in a simpler time, medicine was provided by independent individual practitioners. The physician made all the decisions unfettered by the wants, desires, influences, and decrees of other entities. Over time though, more and more of medicine is being structured. We have coalesced into groups that standardize care. Hospitals introduce protocols and pathways to reduce variability. Insurance companies limit the medications we can prescribe. Consumers rate us on how we're doing. We make fewer free decisions. And in return (or perhaps this takes the analogy too far), doctors, hospitals, and health care institutions develop a common language, a shared set of expectations, and better cross-talk and communication. A lot of older practitioners don't like this; "we know better," they think (and they certainly might). But the newly minted physicians, used to this, appreciate the advantages of common standards and practices. We don't want to separate. We like globalization. And we see it to be the future; the world is more and more interconnected. There are fewer pockets of local isolation and provincialism. To practice medicine, we must meet a global standard. We don't discount that history and legacy that got us here; we look forward to see where things are going.
Wednesday, July 13, 2016
ICU Nursing Care
The intensive care unit isn't just about ventilators and pressors and invasive monitors. Some patients go to the ICU simply because they need the nursing care provided there. Our specially trained critical care nurses are the ICUs greatest asset. I rely on them a lot as they know their patients incredibly well, spending all their time with just one or two. They also develop sharp clinical acumen and great familiarity with the hospital system. I never discount the contribution of our nurses, respiratory therapists, physical and occupational therapists, nutritionists, and pharmacists in the care of our critically ill patients.
Some patients, like those who get a carotid endarterectomy, go to the ICU simply for close nursing monitoring. These patients who have their carotid vessels cleaned out are at high risk for postsurgical strokes. Only our ICU nurses are able to do complete neurologic exams every hour. If the patients do well, they go home straight from the ICU. Other patients come because our nurses can give medications that are restricted elsewhere. I admitted a pre-eclamptic patient to the ICU after her delivery because she needed aggressive blood pressure control that could not be achieved on the regular postpartum floor. Other patients who have complex plastic surgeries may come to the unit for wound care and free flap checks.
Although I enjoy caring for these patients, they are in the ICU more for the nurses rather than the physicians. It is another reminder of the central importance of nurses to our health care systems.
Some patients, like those who get a carotid endarterectomy, go to the ICU simply for close nursing monitoring. These patients who have their carotid vessels cleaned out are at high risk for postsurgical strokes. Only our ICU nurses are able to do complete neurologic exams every hour. If the patients do well, they go home straight from the ICU. Other patients come because our nurses can give medications that are restricted elsewhere. I admitted a pre-eclamptic patient to the ICU after her delivery because she needed aggressive blood pressure control that could not be achieved on the regular postpartum floor. Other patients who have complex plastic surgeries may come to the unit for wound care and free flap checks.
Although I enjoy caring for these patients, they are in the ICU more for the nurses rather than the physicians. It is another reminder of the central importance of nurses to our health care systems.
Sunday, July 10, 2016
Violence and Tragedy
Over the last few weeks, there have been several appalling and unbelievable acts of violence. Incidents like Orlando, Dallas, Baton Rouge, and Falcon Heights have become terrifyingly common. Our emotional responses to them are becoming muted. Our communities are battered. Our values are becoming fractured. Our nation struggles to understand race, sexual orientation, poverty, law enforcement, protest, and anger.
I think it is a medical epidemic. There are outbreaks of violence; each act of violence can infect others to crave retribution. Each act of violence decimates a community. The physical, mental, and emotional scars persist. Physicians, who care for the health of a community and its constituents, ought to respond. We care for those who are victims of child abuse or domestic violence or elder abuse. This kind of violence is not so far off.
In 2011, a Florida law stated that medical professionals should refrain from asking about firearms and not put such information in the medical chart unless it is relevant to the patient's medical care, the patient's safety, or the safety of others. There is no doubt in my mind from what has happened in the past few weeks that this information is entirely relevant to the safety of our communities. We ought to know. We should also know the resources out there to mitigate the risk of gun violence. We ought to educate, support reform, and be role-models to avoid such tragedy. The world cannot go on like this.
I think it is a medical epidemic. There are outbreaks of violence; each act of violence can infect others to crave retribution. Each act of violence decimates a community. The physical, mental, and emotional scars persist. Physicians, who care for the health of a community and its constituents, ought to respond. We care for those who are victims of child abuse or domestic violence or elder abuse. This kind of violence is not so far off.
In 2011, a Florida law stated that medical professionals should refrain from asking about firearms and not put such information in the medical chart unless it is relevant to the patient's medical care, the patient's safety, or the safety of others. There is no doubt in my mind from what has happened in the past few weeks that this information is entirely relevant to the safety of our communities. We ought to know. We should also know the resources out there to mitigate the risk of gun violence. We ought to educate, support reform, and be role-models to avoid such tragedy. The world cannot go on like this.
Friday, July 08, 2016
Always Learning
In a community hospital with a high volume of deliveries, it's easy to get complacent about obstetric anesthesia. For the most part, the procedures are straightforward; we do hundreds of epidurals for labor and spinals for Cesareans a year. There are certainly red flags for those that might be challenging - the patient with severe scoliosis or multiple back surgeries - but the vast majority of women are otherwise healthy, and getting an epidural or spinal is no problem.
I'm always learning though. Several months ago, I was doing the anesthesia for a patient getting a repeat C-section. Her prior C-section happened in a different country and she said she had a spinal which "didn't work." She had so much pain, they had to "put her out." Nevertheless, spinal anesthesia is still the preferred anesthetic for a Cesarean, and after talking to her, we decided to attempt it.
I placed the spinal smoothly in my first attempt; I got back clear CSF, which in nearly all cases, confirms the placement of the medication and the efficacy of the anesthetic. Her response, however, was unusual. She developed a patchy spinal block; there were parts of her leg and abdomen that were completely numb, but other parts that retained normal sensation. This occurred on both sides and at multiple levels; I could not explain this anatomically. We did not have adequate coverage for anesthesia, so I offered to do an epidural. I did not want to do a second spinal because overdosing someone with a spinal can be life threatening. Placing an epidural catheter, however, would allow me to carefully titrate the level of the block.
Again, the epidural went smoothly; the procedure itself suggested it would work well. Nevertheless, as I bolused medications into the epidural, she continued to have a patchy block. After speaking to her and the surgeon, we decided to convert to a general anesthetic. Fortunately, it was in well-controlled conditions; the baby was delivered within two minutes of intubation, there were no problems, and at the end, she awoke to the sounds of a healthy baby's cries.
Even if 99.9% of anesthetics are simple, straightforward, and easy, we will still run into that unusual presentation or odd case that baffles us. Nevertheless, we draw on our education and training, our problem-solving and critical thinking, our knowledge of anatomy, physiology, pharmacology, and medicine, and our skills developing a strong patient-doctor relationship in order to tackle these challenges when they present themselves.
I'm always learning though. Several months ago, I was doing the anesthesia for a patient getting a repeat C-section. Her prior C-section happened in a different country and she said she had a spinal which "didn't work." She had so much pain, they had to "put her out." Nevertheless, spinal anesthesia is still the preferred anesthetic for a Cesarean, and after talking to her, we decided to attempt it.
I placed the spinal smoothly in my first attempt; I got back clear CSF, which in nearly all cases, confirms the placement of the medication and the efficacy of the anesthetic. Her response, however, was unusual. She developed a patchy spinal block; there were parts of her leg and abdomen that were completely numb, but other parts that retained normal sensation. This occurred on both sides and at multiple levels; I could not explain this anatomically. We did not have adequate coverage for anesthesia, so I offered to do an epidural. I did not want to do a second spinal because overdosing someone with a spinal can be life threatening. Placing an epidural catheter, however, would allow me to carefully titrate the level of the block.
Again, the epidural went smoothly; the procedure itself suggested it would work well. Nevertheless, as I bolused medications into the epidural, she continued to have a patchy block. After speaking to her and the surgeon, we decided to convert to a general anesthetic. Fortunately, it was in well-controlled conditions; the baby was delivered within two minutes of intubation, there were no problems, and at the end, she awoke to the sounds of a healthy baby's cries.
Even if 99.9% of anesthetics are simple, straightforward, and easy, we will still run into that unusual presentation or odd case that baffles us. Nevertheless, we draw on our education and training, our problem-solving and critical thinking, our knowledge of anatomy, physiology, pharmacology, and medicine, and our skills developing a strong patient-doctor relationship in order to tackle these challenges when they present themselves.
Tuesday, July 05, 2016
Sugar Sweet
One thing that occasionally interests physicians is seeing the extremes of human physiology. The body can generate and withstand really remarkable perturbations, and from time to time, I am simply amazed by the patients I'm caring for. The last time I was in the ICU, I saw a diabetic patient with a glucose of 1700, 17 times normal. He had hyperosmolar hyperglycemic nonketotic coma, which we like to abbreviate "HHNK" (with various spellings). He had been unconscious for days, likely from an infection, and meanwhile, without his insulin, his glucoses became completely out of control. He came in extremely cold, profoundly dehydrated, and unresponsive. Yet after a day and a half in the intensive care unit, by the time we got his glucoses down to 200, he returned to his usual normal self. He left the unit the next day and returned home several days later.
This is by no means an unusual or even difficult intensive care unit case. But when I think of it, I pause because there is something simply ineffable about the resiliency of the human body. Most of the medicine that we practice is aimed at getting the human body back to its baseline homeostatic state.
This is by no means an unusual or even difficult intensive care unit case. But when I think of it, I pause because there is something simply ineffable about the resiliency of the human body. Most of the medicine that we practice is aimed at getting the human body back to its baseline homeostatic state.
Friday, July 01, 2016
The Capacity to Change
We underestimate our capacity to change. When I talk to a lot of my friends who are physicians, I hear stories about those who frustrate us: the parents who don't believe in vaccination, the uncle who continues to smoke, the roommate who "doesn't believe in taking medications." We see patients who are addicted to drugs, who drink themselves into liver failure, who won't check their blood sugars, who ride their bikes without helmets. But I think we underestimate the human capacity to change.
We do this for ourselves too. We don't think we can adhere to a new diet, we give up on our exercise goals, we let our projects waste away. And we think that's par for the course. We encourage others to change without meaning it. We make resolutions we know we won't keep. We go through life half-hearted and unmotivated.
I don't think it needs to be this way. I have seen true, genuine change. I have seen people's values, principles, ethical stances, political positions, and convictions change, adapt, and renew with time. I have met that cancer patient who quit their long-time job to write a book about dying; I know the chemical engineer who gave up that life and now meditates for fourteen hour sessions on the weekends; I have treated the investment banker who became an art philanthropist; I have talked to the abuse victim who confronts her abuser.
We need to expect change of ourselves. Change is a natural process of the self-aware life. When we live an unexamined life, when we stop questioning who we are and why we do things, we get into a rut and wither a little. When we need others to change, we are right to expect it of them, and we are also responsible for helping them reach it. In reflecting on our lives and what we expect from ourselves, we hope to become clearer and truer to our convictions, our goals, our values, our friends, our family, our community, and ourselves.
We do this for ourselves too. We don't think we can adhere to a new diet, we give up on our exercise goals, we let our projects waste away. And we think that's par for the course. We encourage others to change without meaning it. We make resolutions we know we won't keep. We go through life half-hearted and unmotivated.
I don't think it needs to be this way. I have seen true, genuine change. I have seen people's values, principles, ethical stances, political positions, and convictions change, adapt, and renew with time. I have met that cancer patient who quit their long-time job to write a book about dying; I know the chemical engineer who gave up that life and now meditates for fourteen hour sessions on the weekends; I have treated the investment banker who became an art philanthropist; I have talked to the abuse victim who confronts her abuser.
We need to expect change of ourselves. Change is a natural process of the self-aware life. When we live an unexamined life, when we stop questioning who we are and why we do things, we get into a rut and wither a little. When we need others to change, we are right to expect it of them, and we are also responsible for helping them reach it. In reflecting on our lives and what we expect from ourselves, we hope to become clearer and truer to our convictions, our goals, our values, our friends, our family, our community, and ourselves.
Subscribe to:
Posts (Atom)