Sunday, May 31, 2009
Poem: About Suffering They Were Never Wrong
-
About Suffering They Were Never Wrong
In this closet of a room, bisected from stem to stern,
one side tumbling with string, tied to ants and not,
seashells and the echoing ocean,
cones of conifers and pelts of beach-strewn animals,
feathers and feathers, some plastered with glue,
a discarded belt with a rash boy's blood,
hourglasses and spectacles and magnifying lenses
by which we spy blueprints and landmarks,
statues of Athenian children to be sacrificed
to some God dethroned, black sail and bride.
The other half, a bed made with pillows fluffed,
a doll tucked under the blankets, cataracts blooming in its eyes,
a stool and a desk, marbles in their leather bag,
wooden toys lined up, soldiers carefully arranged
with shield and spear in a phalanx,
the sun shining through the only window in this tower of legend,
and on the sill, a small footprint in the dust to indicate
where they jumped, the only impulse this side of the room
which prompted Minos himself to ask
how come it was the one who made it, not the other.
Saturday, May 30, 2009
Drowsiness is Red Alert
Long hours are necessary; I'm resigned to that. While some specialties like emergency medicine and anesthesia are shift-based, I'm not sure if traditional inpatient disciplines like medicine or pediatrics translate as well into such paradigms. There is something to be said about working a new patient up and being a part of their care for the first 12-24 hours. That's when all the action happens. That's when the critical decisions are made, the initial results come back, and the plan of action is determined. The educational value in this cannot be underestimated; house staff learn how to manage patients by seeing the results of the choices they make. The problem with shorter shifts is that you hand-off your patients without seeing the results of your plan or you get patients whose plans are determined by their previous providers.
So then it becomes the balance between fatigue and handing off patients. In my last call night, I didn't sleep at all, and I feel that for me, fatigue does play a role. My thinking is slower, the justifications for my decisions less complete, my reaction time prolonged. I have to addend my presentations after I finish them because I forget a key component and my notes are either rambling or too sparse. I take circuitous routes around the maze that is SFGH rather than the shortcuts. I'm tired and my head hurts.
As I get more efficient, as straightforward things become more reflex than cognition, as I solidify confidence, I'm sure things get easier. I can build my endurance, learn to steal those precious moments of rest, multitask better. But I think in the end, there is a limit to how good someone can be when they are exhausted. The key is to find the balance between that and the risks one takes when patient care is handed off from one person to another.
Thursday, May 28, 2009
S2
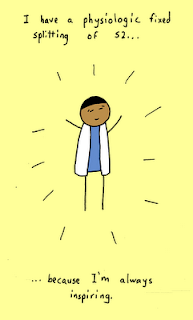 I wish I thought of this medical pun.
I wish I thought of this medical pun.Image is shown under fair use, from "Cowbirds in Love" drawn by Sanjay Kulkarni.
Tuesday, May 26, 2009
Life at the General
Some of the attending teaching rounds for this rotation have given me weird flashbacks of first and second year. My attending is really into hands-on visual learning so we took field trips down to the hematology and microbiology labs. With hematology, we reviewed peripheral blood smears, looking at sickle cell anemia, schistocytes, plasmodium falciparum, and chronic myelogenous leukemia. For a whole year now, I've relied on reports ("1+ polychromatophilia, 1+ ovalocytes") and I've lost touch of how beautiful (yes) blood smears really are. It's quite fun hunting for that wayward basophil or deducing multiple myeloma from rouleaux.
But even more fun was the microbiology. This gave me flashbacks to my summer working on Pseudomonas, that blue-green queen of rods. The smell, the agar, the gram-stain apparatus across the sinks were all quite reminiscent of micro lab. Remember optochin? How do you calculate MIC? We looked at slides and plates. It was fun.
Though we won't be experts at hematopathology or microbiology, having a sense of what thinking goes into such disciplines is important. It's too easy to read report conclusions and forget how much expertise goes into interpreting smears or slides. I do think it would be fun to do gram stains at the bedside, but alas, such days are gone.
Yes, my laboratory tests are still pending.
Monday, May 25, 2009
My Sister's Keeper
 Yes, I have been able to read for fun. I recently finished My Sister's Keeper by Jodi Picoult, a mediocre book based on a fascinating premise. This is a book about two sisters, the older one with leukemia and the younger one conceived for her umbilical cord blood to save her sister. The older sister is dependent on the younger for her health. How does this change their relationship? How does it change family dynamics? I can't be too sure of the science but I read it for leisure. In many ways, it ends up being too sensational, too "pop" for me. It has that "written to be a best-seller" feel, but it's an easy read, amusing, thought-provoking. It's not a "must-read" but could be worthwhile for someone with the time.
Yes, I have been able to read for fun. I recently finished My Sister's Keeper by Jodi Picoult, a mediocre book based on a fascinating premise. This is a book about two sisters, the older one with leukemia and the younger one conceived for her umbilical cord blood to save her sister. The older sister is dependent on the younger for her health. How does this change their relationship? How does it change family dynamics? I can't be too sure of the science but I read it for leisure. In many ways, it ends up being too sensational, too "pop" for me. It has that "written to be a best-seller" feel, but it's an easy read, amusing, thought-provoking. It's not a "must-read" but could be worthwhile for someone with the time.Image shown under fair use, from www.nassaulibrary.org.
Sunday, May 24, 2009
Poem: Trichotillomania
-
Trichotillomania
Ever since I came to this house,
my hair has fallen out. The janitor
knows where to find me,
sweeping curls every day
a trail leading to my room
another tuft between my fingers.
Looking in the mirror each morning,
the voices say, this is the moon
and this is your head,
see how it must shine?
Some days I pull, not to appease the voices
but to sniff them out, hunt them down
hiding somewhere beneath my scalp
playing peek-a-boo in my brain.
The men in coats look concerned
when I tell them
and they exchange one pill for another.
I cloister them in my cheek
and spit them out when they leave
because the truth is
I like being a monk
living in this sanctuary
hearing my prayers rebuffed
by voices I cannot satisfy.
Saturday, May 23, 2009
Placement and Dispo
In my rotations at SFGH, I've noticed how difficult "dispo" (disposition, that is, post-hospital plan) can be. On neurology, we had patients who had been in the hospital for a year without acute medical necessity simply because their insurance status doesn't allow them to go to the type of nursing facility they need (they had a tracheostomy which can be cared for at some skilled nursing facilities, but none that took their insurance). On our service now, we have patients who are undergoing the weeks-long process of being conserved (appointing a legal decision maker because their illness makes them incapable of making medical decisions). We have a patient who has too much money to leave the hospital (I'm not sure of the exact details, but he has mutual funds or bonds that he won't liquidate and he can't leave the hospital to a Board and Care until he qualifies for Medi-Cal). We have a patient from San Jose who is waiting for a bed down there to be transferred. The social workers, case managers, and utilization review here are fantastic, but the challenges are immense.
Friday, May 22, 2009
Call
My first call cycle wasn't too bad; I admitted a comfort care patient, a community acquired pneumonia (rule out TB), and an ICU transfer of a patient recovering from presumed Still's disease flare (that's almost a Moffitt case). We were "slammed" early on; the interns were in clinic and we got six or seven admits by early afternoon. On the other hand, my second call cycle had an almost unheard of lull; our team as a whole only admitted one patient (perfect for the third year student) and I didn't get any. I spent most of my time catching up on my work and indeed, writing blogs.
Thursday, May 21, 2009
First Call
My first patient on medicine was a man with acute on chronic pancreatitis. There were some unusual aspects to his presentation with a surprising transaminitis (AST 3000), but one particular incident stands out in my mind. We were sending daily labs and one day the lab pages me with "critical lab values," tests that are so abnormal that the laboratory must call the nurse and MD to confirm we got the results. I was told about a potassium of 2.8 and low calcium, but when I reviewed the lab results, I was shocked to notice a four point hematocrit drop (which wasn't "critical" by lab standards but the most worrisome value for me). The crit drop suggested he was bleeding. I quickly paged my resident and went to see the patient.
The patient was gone. I couldn't find him. I talked to his nurse who said that he left the floor for a cigarette break (despite being counseled to quit smoking and drinking) and had been gone an hour. We overhead paged him and sent someone to look for him, afraid that he was missing with a critical lab value and would be found unconscious somewhere. It was my second day of fourth year and I had lost my patient.
In the end, he returned from his smoking break and the lab values turned out to be spurious (dilution effect because it was drawn from the same arm that was receiving IV fluids). But this was a scary reminder that being first call, I have to be ready for anything.
Tuesday, May 19, 2009
Sub-I
Being a sub-intern comes with all the administrative baggage. I have to call for outside records, fax prescriptions to the pharmacy, dictate. Dictations are really hard for me. I had to do them in surgery, but those dictations were more straightforward. On medicine, patients come with an extensive problem list and figuring out how best to communicate them is difficult but very educational.
The other new thing is doing sign-out. Sign-out is an immensely important process by which a patient's care is transferred from one person to another. At the end of each day, I have to sign out my patients to the night float (who's in the hospital overnight) or the cross-covering intern (harder to explain). I need to anticipate any problems the patient might have and put down any to-do's for the covering resident. This requires thinking through all the patient's problems and anticipating the worst case scenario. What should the night float do if the patient spikes a fever or drops his blood pressure or becomes combative? After participating in this process of sign-out, I realize how critical it is to efficiently transfer information about a patient to someone who has to learn about dozens of people in a short period of time.
Monday, May 18, 2009
Inspiration
Sunday, May 17, 2009
Fiction: How To Die
How To Die
First, I take off my skin. I peel it from my body like a film off a delicate dessert. It doesn’t come easily but with a little persuasion, I get my arms out of these sleeves and wriggle, my skin falling away like a slip at my feet. I pick up this hula-hoop of flesh, shake out the folds, and set it onto a coat hanger lest it get more wrinkled. With my skin off, I realize how much lighter I’ve become.
I dance. I’ve never learned to dance, but now that I’m dying, it’s time. My daughter teaches me to pas de basque. I feel the floor for the first time in years. As I glissé, my feet slide along the grainy wood, and as I sauté, the sprung floor responds. I’ve had trouble learning new things, but this comes naturally. Watch one, do one. I ask my daughter, "What is the pas de basque?" and her eyes become verdant in a way I’ve never noticed. She tells me of the 19th century Bialy Mazur, of petticoats and elbow length gloves. We dance through the rooms together, and as my feet skip along the grain, I imagine the horses of the Polish cavalry racing in waltz time across the steppes of Central Europe.
My heart begins to quiver, whistling to the music in my head with remiss and unaware frankness. This is the last dance, the last chance for those all-night ball-goers. They dance fiercely. I look down at my chest, see my heart glisten through the ribs. Each time it squeezes, it looks like it's winking. You might ask: how could I see my heart? Did the muscles between my ribs come off with the skin? I don’t know, but today I don’t worry. There are many things that have left my mind like whether I have my hair or whether my daughter is still dating the guy at the bowling alley. That thought quickens my pulse. I turn to say something, but when I see her eyes, I can’t. They're green, still. Instead, I ask her to turn off the lights as she leaves the room so I can lie down and reach behind the whispering and tremulous organ to loosen its screws.
Saturday, May 16, 2009
Fourth Year II
It is an inculturation of sorts. We learn what things are important in clinical medicine, and most of the time, they are in stark contrast to textbook medicine. Patients' insurance status matters. The day of the week is important. Horses, typical or atypical, far outnumber the zebras, even in a tertiary academic institution. We learn how to work in teams, work with patients, work as students. How do you introduce yourself to a patient when it's your first day on the rotation? Half the parents knew more about childcare than I did. But I learned to identify my place in this confusing spiderweb of health care delivery.
Over the year, I've been gathering more and more responsibility like a rock rolling down a hill. But a third year clerk always has the option to sit and watch if we don't feel comfortable with things like calling a consult, delivering a blue baby, or running a family meeting. But as I look ahead to fourth year, I'll be expected to do those things, difficult in different ways. It's like taking one of the training wheels off; I'll be okay for the most part, but a steep hill is really the test. I'm feeling pretty apprehensive but I have some measure of confidence that I can manage the learning curve. Everyone says that fourth year past the sub-interships is a great year; it's a breath of relief between the grind and rigor of third year and internship, and hopefully I'll take advantage of that.
Friday, May 15, 2009
Fourth Year I
At the end of third year, I feel good. I survived. It's supposed to be the "hardest" year, and I enjoyed it. It was great going into a rotation knowing absolutely nothing yet coming out knowing something. The people I worked with loved to teach and try to get us to go into the specialty. I saw open heart surgery, I delivered babies, I had one woman ask me to be her primary care doctor. I saw what it was like to be incarcerated or paralyzed or schizophrenic or a parent. Moments like that make all the interim worth it. It was not easy, and I would be wrong to pretend it was. There were distinct hours, days, weeks when I wished I was doing something else. I floundered. I had no confidence in myself. I thought about running away and writing the next great American novel or joining a band.
I've changed. The transformation is quite remarkable yet I don't notice it until I reflect. For one, naked people don't bother me (the confounder, of course, is living in San Francisco; Bay to Breakers is this weekend). Seriously though, I have more confidence than when I started; I wear my white coat rather than let it wear me. I feel more a doctor than an imposter, and while that is an expected change, I struggle to prevent myself from adopting bad habits. I try to preserve humility, empathize with patients, and ignore the clock. After a year on the wards, I've learned to think on my feet. I remember the beginning of third year when my routine was to see a patient, rifle through my handbooks trying to figure out what the patient has, google, wikipedia, or UpToDate the disease to figure out what tests and treatments I would need, and finally present to a preceptor. My rate was two to three patients an afternoon clinic. Now, I find myself more comfortable juggling multiple patients simultaneously, thinking on the fly of what I want, and relying more on my "fund of knowledge" rather than external sources. I can hear presentations of other patients and feel the cogwheels in my head turning, trying to figure out what is going on.
Wednesday, May 13, 2009
Fourth Year Scheduling
My fourth year is front-loaded beginning with sub-internships in internal medicine and intensive care. Then I have two weeks of dermatology and two weeks of palliative care. Late in the summer, I do months in infectious disease and cardiology. By October, my schedule becomes a lot lighter. I spend a month doing a lecture-based class on clinical therapeutics. I plan on teaching first year medical students (cardiovascular block) in November and December during interview season. In January, I have a month of pediatric cardiology followed by emergency medicine and radiology. I also have an extra month floating around there which will probably be vacation. The only other rotations I might add in later would be EKG, pulmonary, ophthalmology, hematology, rheumatology, nephrology, or endocrine. As a whole, I got what I wanted and it works well for both a medicine or anesthesia track. Nearly all my rotations are at San Francisco General Hospital; I'll miss the ivory tower of Moffitt and the beautiful coast of the VA. I wish I had more VA rotations, but I can't really complain.
Tuesday, May 12, 2009
The Physician Workforce
Interestingly, the COGME 16th report 2005 indicates the physician supply is slightly increasing; in 2000, there were 283 full time equivalents per 100,000 people, in 2005 there were 293 full time equivalents per 100,000 people. But as you would expect, the number of generalists has stayed fairly constant since the 1960s while the number of specialists has trended up. It's hard to estimate whether there's a shortage or surplus of physicians; how do we know what an ideal patient panel is for a primary care doctor? Do we use traditional economic forces of supply and demand to understand the various forces on the physician workforce? Furthermore, disparities are highly regional. Even in California, highly physician populated areas (the bay area, Los Angeles, Orange County) are next to areas with few physicians (inland empire, central California).
Yet the supply of physicians has stayed relatively constant; since 1980, the annual number of graduates of U.S. allopathic medical schools has been stable at 15-16,000. These make up 2/3 of residents; in 2005, international medical graduates made up 26% and osteopathic graduates made up 12%. Fewer and fewer internal medicine residents are choosing careers as generalists; in 1998, over half of residents wanted to be generalists while in 2005, only 20% did (Bodenheimer, NEJM 2006).
One can also analyze the supply in many different ways; the number of women and minority physicians is increasing. The empirical evidence suggests that to serve minority populations, we ought to train minority physicians, so this is an effective trend. In the end, I'm not sure how to interpret all this data. I think it would be difficult but helpful to expand medical school classes and start new medical schools, especially in areas with underserved populations. I think we need to turn more to allied health professionals like nurse practitioners and physician assistants to help fill primary care since the trends suggest making more physicians would lead to making more specialists.
Sunday, May 10, 2009
Revision: Life and Death in the Hospital
I took two poems I wrote last year and merged them into this poem in an attempt to contrast the two very different scenes I witnessed.
-
Life and Death in the Hospital
Her hair, cut in the style of a Japanese pop star,
a prevenient wild, pulling your attention
from the brewing storm, the nurses frantic.
Given the name Giraffe as she rolled through emergency,
I wondered about her identity.
What TV shows did this eight year old like?
Who were her friends? Did she like giraffes?
Ever since she was two, we knew the course;
what did the last six years mean,
how did her parents turn that corner?
An anime face, her pupils wide and doll-like
comforting to those who knew the least
who held her hand and bridged the chasm
rolling polka-dot socks onto her feet.
Up in labor room six, a Berkeley grad dances
nude, her belly flowing from corner to corner
shiny as the full moon. She feels rhythm
in her contractions, gives the anesthetist a wink
and turns up her iPod, a new age jazz.
Twirling, clothes strewn, prancing
in no particular manner but beautiful.
I imagine her baby, heart at a hundred twenty,
bouncing to an amniotic fluid samba
signing a lease out of confinement
into that embrace of sunlight
or at least, the San Francisco fog.
Saturday, May 09, 2009
Dawn Mazur
The Dawn Mazurka is an old tradition that died out and was resurrected at Stanford Big Dance. It comes from the Polish Mazur, but as several countries conquered Poland in the 18th and 19th centuries, it was adopted and adapted by Russia and the Germanic empires. In any case, after many iterations, one Russian Mazurka Quadrille emerged as the ultimate challenge for 19th century dancers, choreographed by a Charles Durang in 1856. At all-night balls, this complex partnered set dance was done at dawn as the hardest dance when people were most tired. We dance a reconstruction by Richard Powers at around 5AM, and it's fantastic. Then we always follow it with the Chicken Dance.
Friday, May 08, 2009
Intersession
Much of intersessions also prepared us for fourth year and beyond. There were several panels discussing how to deal with ethical dilemmas and medical mistakes. We reviewed common bugs and drugs, radiology basics, and EKGs. We finally got a formal lecture on common ICU problems, ventilator settings, and the importance of sign-out. We listened to heart sounds and practiced putting IVs in each other. In small groups, we looked at the basic science and clinical trials of the human papilloma virus and the new Gardasil vaccine. It's interesting; in actually reviewing the data, I would recommend it for an appropriate individual (someone with minimal exposure to HPV), but I would be hesitant to recommend it for a population (I am unconvinced the cost-benefit analysis for populations is as favorable as it is for an individual).
For career development, many specialties had information sessions, and we learned about putting together CVs and personal statements. It's all a little overwhelming, but I guess I'll take the process as it comes. In any case, it was really fun seeing all my friends, refreshed and ready. I loved meeting again with my Foundations of Patient Care small group and hearing what everyone wants to do. It's amazing that for many of my classmates their plans and passions have solidified. Hopefully now I'm ready to tackle fourth year.
Thursday, May 07, 2009
Wednesday, May 06, 2009
Tuesday, May 05, 2009
Decisions V
I am really 50-50 at this point. I fear that if I go into internal medicine, there's a chance I'd do a second anesthesia residency after that (maybe a 20% likelihood). While it's not uncommon, it's certainly not ideal to do two residencies and my goal is to minimize that likelihood by committing now.
My first two rotations as a fourth year medical student will be sub-internships, intensive inpatient clinical experiences. I begin with internal medicine at San Francisco General Hospital where I will act as the intern (first year resident) with the associated responsibilities. This is followed by a month in the intensive care unit at SFGH (the recommended anesthesia sub-internship). Hopefully after these two rotations I will have figured out what I want to do. Early in my fourth year, I will also do a month of cardiology and infectious disease, and that will help too.
Monday, May 04, 2009
Decisions IV
What really got me was clinical problem solving; I even bought a book of NEJM cases. I absolutely love that strange idea of taking a story and figuring it out. That thought process fascinates me; how do we learn to do pattern recognition? How do we figure out what a diagnosis is? I got so wrapped up in the differential diagnosis that I even made a website for my own learning (http://caseoftheday.blogspot.com/) and still take two hours each weekend reading more. That feeling when a case clicks and all falls together is addicting and intoxicating. And clinical problem solving is far more than that: I like learning about the sensitivities and specificities of signs, symptoms, and tests; I like framing these questions in terms of pre-test and post-test probabilities.
My favorite third year rotation was medicine. I loved the sick inpatients, the acuity, the diversity of diseases, the mystery cases. I loved the EKGs, the chest X-rays, the physical finding rounds. My attendings and residents impressed me so much with their finesse and deduction. Then they turned around and told me I should do medicine as well; they seemed to recognize in me some unbeknownst talent.
There are aspects of internal medicine that give me pause. My dad warns me that general internal medicine as a practice is not as fun as it seems now; common things are common and the bulk of the work is not all that intellectually stimulating. I also think management is a plus-minus; although it's certainly important and fundamental to medicine today, I could be just as happy in an Oslerian world were we diagnose things but have little to offer. Medicine offers a wide range of specialties, including those that are procedural and interventional, those that are completely cognitive, and those that are in between. It is almost like delaying a decision on what kind of doctor I want to be. At this point, I think the most interesting fields would be cardiology (especially clinical cardiac electrophysiology) and infectious disease.
Sunday, May 03, 2009
Poem: Sound
The first double-stop arrests my heart.
A flutter, a glissando, a prickling of hairs
when he puts that violin to his chin,
the grain of the wood worn down
like an old man's face.
I expect a doddering,
an Alzheimer's cry to come from
that fragile instrument
but instead he belts out Bach's Chaconne
Partita No. 2 in D minor.
D minor! Who could have said
listening to the lilting waves, the rich belly
that cracks open wallets
and stone hearts?
He moves across the stage,
his arms, torso, head and neck fiercely
defending the melody.
Bullets of sweat fall from his face
barely missing the fingerboard,
the scroll of the violin
dancing in arcs and furies
the bow in pirouettes and plies
the audience held
by golden fetters, diamond shackles.
Saturday, May 02, 2009
Decisions III
At UCSF, I worked with an extraordinarily accomplished anesthesiologist on Pseudomonas infections. Her training was pretty crazy; she went into medicine, followed by a pulmonology and critical care fellowship, then went back and did anesthesia. Her experiences have convinced her that anesthesia was the route to take. In my first two years, I poked in and out of different anesthesia related events, meeting different faculty and residents, doing some shadowing in the operating room. I liked it; I liked the procedures, the back-seat role (as opposed to the surgeon), the focus on vigilance. When I did other rotations, I had more than one resident tell me to do anesthesia, mostly because of the lifestyle. When I did my anesthesia rotation, it was as I expected. Many of the cases were a little boring after induction, but the cardiac cases were super exciting. I enjoyed doing the hands-on stuff, but I wasn't great at it. I felt there was a little less patient interaction than I would have wanted but more than I expected. Working with surgeons is a plus-minus. But the anesthesiologists themselves were great.
My personality fits anesthesia. I like things that are scheduled and structured. I like having control. When I worked in a basic science lab, my bench was always neat and organized. Things had their place. They were labeled with concentration, expiration date, initials. I thought through my experiments and what I'd do when they failed. Anesthesia is like that; it's a specialty for planners, and a lot of the cognitive weight is built into that aspect. I like finishing one thing before starting another.
The material is interesting to me. I think I will like critical care medicine, its complexities, and its gravity. I like managing multiple drips, large volumes of data, and an evolving process whether surgical or in the ICU. Physiology and pathophysiology are great, and pharmacology, insofar as anesthesia is concerned, seems doable.
The training is reasonable. It offers further specialization into critical care, pediatric, and cardiac. Pain is available if I decide I want more longitudinal continuity with patients. The lack of patient continuity bothers some people. It might bother me, but I'm not sure yet. And I cannot downplay the lifestyle; the pay is good, the hours are somewhat flexible, and it's on that enviable "ROAD to success" (made up of radiology, ophthalmology, anesthesiology, dermatology).
Friday, May 01, 2009
Decisions II
The next step - surgical or nonsurgical - is also easy. I don't like surgery enough to commit to it. Surgery is fun; it's hands on, interventional, and technically challenging. It can be rewarding to see something wrong and fix it. But it requires a great investment in time and has its culture and preconceptions. I'd miss the cognitive aspects of non-surgical fields.
A related question is whether I want a procedural or non-procedural field. I think it'd be fun to do something procedural but I'm not opposed to doing something completely cerebral. I would include things like anesthesia and interventional cardiology in a short list of interesting fields. There are other benefits to doing something hands-on; as the medical landscape changes over the next few decades, I think allied health professionals (nurse practitioners, physician assistants) may broaden their scope of practice. They may do more of the health maintenance and management of patients, but seem less likely to extend too much into the procedural aspects of medicine (other than nurse anesthetists). By having a set of procedures one can do, a physician better secures his or her area of expertise.
Lastly, looking at patient population, one could ask adults or children. I think I'm an adult-type person, but I wouldn't mind caring for children. Why adults? My answer isn't very satisfying; I simply always imagined myself as an adult doctor. This leads me into a field like medicine but fields that do both adults and children like emergency medicine might be fun too.





