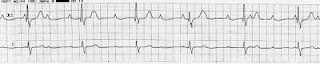
On one of my recent call days, I cross-covered a patient with a profound cardiac dysrhythmia. The primary team had been trying to control a rapid heart rate: atrial fibrillation with rapid ventricular response, but had been unsuccessful for several days. Finally, they came upon a cocktail that worked: high dose long acting diltiazem, moderate dose metoprolol, and a touch of digoxin. In the clinical years, we learn that you never use two nodal blocking agents at once; that is, never put a patient on two drugs that slow the cardiac conduction through the atrio-ventricular node because it has too high risk of completely blocking the conduction through that node. Here, the patient required three separate nodal agents. She then became bradycardic with a number of different rhythms captured: a sinus bradycardia, an idioventricular rhythm, a junctional escape rhythm. But she looked stable for the time being and the team put pacing pads on her just in case.
As the on-call intern, I cross-covered the patient - meaning that I took care of her after the primary team left the hospital. I got ominous pages from the nurse and each time immediately saw the patient as I knew she was a high cardiac risk. She was always asymptomatic, but occasionally, her heart rate hovered in the high 30s. Finally, I witnessed something overwhelmingly terrifying: prolonged pauses between heart beats. If you think of the normal heart beat as 60-100 times a minute, a heart beat should go by at least every second. Here, the patient was having up to 4 second pauses before her heart would beat again, a true indication for a pacemaker.
Watching her and listening to the monitor was one of the scariest moments that call day. I could feel my heart skip as I listened for the next heart beat, worried it may never come. I started initial pharmacologic treatment: calcium gluconate to reverse the diltiazem and atropine. Finally, her eyes rolled back and she stopped responding, and we had to call a code blue and start pacing her transcutaneously. Luckily, everything was all prepared and we didn't have any problems. But it was one of the scarier codes where I was the first responder and had to determine the appropriate initial plan of action.
Image of complete heart block from Wikipedia, in the public domain.



No comments:
Post a Comment