Sunday, July 31, 2011
Medicine in the Operating Room
Sometimes anesthesia is characterized as "medicine in the operating room," and this is not far from the truth. While much of anesthesia is intubation, etc., a lot of it is also a secure understanding of a patient's medical conditions and how the stress of surgery impacts these underlying disease states. For example, many of the veterans I see have a lengthy past medical history, which can change the anesthetic plan. The intubation strategy changes with obesity or reflux disease or a history of neck radiation; the paralytic I choose differs if someone is bedbound or has hyperkalemia or has chronic kidney disease; the emergence changes if someone has severe coronary artery disease and is on a beta blocker. Understanding coronary valve diseases helps me decide intraoperatively how to manage blood pressure and fluid status, and putting someone on a ventilator can be much more difficult if the patient's pulmonary compliance is poor. Anesthesia is about weathering a sick patient with many comorbidities through a surgery where a large incision may be made, an organ resected, and blood lost. I really do think it is the practice of acute care medicine perioperatively.
Saturday, July 30, 2011
Call, and Other Trivialities
Anesthesia's workweek is very different from that of medicine. When I was on medicine, there was little differentiation between weekdays and weekends because patients get admitted to the hospital every day. There are fewer didactic sessions on weekends, but we still make our rounds and take care of our patients. On the other hand, anesthesia is a very weekday heavy specialty. All scheduled surgeries happen on weekdays, and we are available only for emergency operations and airway emergencies on weekends. Because of that, my schedule is pretty heavy Monday to Friday, but fairly light on the weekends. Even when I take in house call, the days tend to be a lot lighter than they were on medicine.
At the VA, we take first and second call several times a week (it is different at other hospitals). Being second call means that we stay until there are only two operating rooms open. Being first call means we stay until the end of the day and remain in house with the airway pager. This call system allows us to have some assurance that we will end at a reasonable time when we are not on call because even if we are assigned to a long surgery, one of the call residents will relieve us at the end of the day.
At the VA, we take first and second call several times a week (it is different at other hospitals). Being second call means that we stay until there are only two operating rooms open. Being first call means we stay until the end of the day and remain in house with the airway pager. This call system allows us to have some assurance that we will end at a reasonable time when we are not on call because even if we are assigned to a long surgery, one of the call residents will relieve us at the end of the day.
Thursday, July 28, 2011
Book Review: The Tennis Partner
 The Tennis Partner by Abraham Verghese is a fairly autobiographical story by my previous residency program director. Part of the reason I chose Stanford for my internship year was because I was drawn to a program whose figurehead was a writer. And indeed, after getting to know him in a professional capacity over the last year, I ventured to seek him out in the literary form. This is the first book I've read of Dr. Verghese. It is a story of his time in El Paso, Texas, where as a young professor of medicine, he befriends a medical student recovering from drug addiction. At the same time, he describes the unraveling of his own marriage. The two of them, at first harbored in isolation, find a bond on the tennis court, developing a relationship of professor-student, friend-friend, and tennis coach-devotee. It is a beautifully written story that explores relationships between friends, lovers, and addictions, the practice of medicine at the border of Texas and Mexico, the history of tennis, and the psychological struggle of drug use, rehabilitation, and temptation.
The Tennis Partner by Abraham Verghese is a fairly autobiographical story by my previous residency program director. Part of the reason I chose Stanford for my internship year was because I was drawn to a program whose figurehead was a writer. And indeed, after getting to know him in a professional capacity over the last year, I ventured to seek him out in the literary form. This is the first book I've read of Dr. Verghese. It is a story of his time in El Paso, Texas, where as a young professor of medicine, he befriends a medical student recovering from drug addiction. At the same time, he describes the unraveling of his own marriage. The two of them, at first harbored in isolation, find a bond on the tennis court, developing a relationship of professor-student, friend-friend, and tennis coach-devotee. It is a beautifully written story that explores relationships between friends, lovers, and addictions, the practice of medicine at the border of Texas and Mexico, the history of tennis, and the psychological struggle of drug use, rehabilitation, and temptation.I really enjoyed the book. I didn't know what to expect, since I knew the author (though he was never my attending), and I found it strange, uncomfortable, then curious to step into his past life where he reveals things he wouldn't otherwise. As I read the book, I heard his voice; the storytelling is a representation of the person I know. The writing is magnanimous; at times, it is too large and tries to swallow too much, but for the most part, he coaxes history, geography, science, psychology, and fantasy into a medley of emotion. I really enjoyed The Tennis Partner and look forward to reading other works by Dr. Verghese.
Image shown under Fair Use, from www.abrahamverghese.com.
Wednesday, July 27, 2011
Education
 Our first month of residency is packed with didactics. They assume we don't know anything and start from the beginning. Orientation involved some simulation exercises. Simulation is the big educational tool in anesthesia now; anesthesia is an ideal field because it involves teamwork, cooperation, crisis management, leadership skills, and communication as well as hands-on skills, quick problem solving, and critical thinking. We also get 2 hours of lecture 3 times a week on basics from pharmacology to physiology to ethics. Lastly, we are supposed to work through an introductory workbook and set of slides. It's really great, though I think my coresidents and I are pretty exhausted.
Our first month of residency is packed with didactics. They assume we don't know anything and start from the beginning. Orientation involved some simulation exercises. Simulation is the big educational tool in anesthesia now; anesthesia is an ideal field because it involves teamwork, cooperation, crisis management, leadership skills, and communication as well as hands-on skills, quick problem solving, and critical thinking. We also get 2 hours of lecture 3 times a week on basics from pharmacology to physiology to ethics. Lastly, we are supposed to work through an introductory workbook and set of slides. It's really great, though I think my coresidents and I are pretty exhausted.Image of Duke anesthesiology simulation shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Tuesday, July 26, 2011
Flexibility
Flexibility is incredibly important as an anesthesiologist. Although we want as much of our work to be pre-planned and anticipated, we also have to adapt quickly when things change. Every day, the operating room schedule for the following day is made. We look up our patients, determine the anesthetic plan, and discuss the cases with our attendings. But invariably, these schedules change up to the moment the patient enters the operating room. Emergency cases get added on. New developments in scheduled patients necessitate further work-up or delay of surgery. Cases go longer than scheduled, and the last case of the day may get bumped. The operating room scheduler has to take into consideration staffing of operating rooms, whether a case is "clean" or "dirty" (for example, replacing an infected hip joint should not precede a fresh total hip replacement), and call schedules. So I've learned that when I come in and am told my room has been canceled and replaced with all new patients simply to roll with it.
Monday, July 25, 2011
The VA
I'm at the VA for my first two months. It's a good place to start. After I got to know it as a medicine intern (I spent a third of the year here), I've realized it's a smaller place than it seems, and the community of physicians here is really easy to work with. I like the patient population; veterans are hardy, candid, encouraging, and gruff. They do come with a complicated past medical history though; many of our vets have hypertension, hyperlipidemia, some measure of coronary artery disease, COPD from smoking, diabetes, obesity, psychiatric comorbidities, and substance abuse. This can make anesthesia difficult; it's harder to secure an airway in an obese patient with poor dentition, it's harder to ventilate someone who's an active smoker with lung disease, and it's more important yet harder to maintain stable hemodynamics in patients with such comorbidities.
In any case, I'm enjoying it. I get in at around 6am to set up my room, draw my medications, and meet the patient at 6:40. I prepare the patient, place the IV, and we're in the operating room a little after 7. The attendings are incredibly supportive and since it's a small group, we have a lot of continuity from day to day. We get a few breaks and most rooms end mid-afternoon. Around that time, I look up my patients for the following day and talk to that attending about my concerns and plans. It's a smooth routine.
In any case, I'm enjoying it. I get in at around 6am to set up my room, draw my medications, and meet the patient at 6:40. I prepare the patient, place the IV, and we're in the operating room a little after 7. The attendings are incredibly supportive and since it's a small group, we have a lot of continuity from day to day. We get a few breaks and most rooms end mid-afternoon. Around that time, I look up my patients for the following day and talk to that attending about my concerns and plans. It's a smooth routine.
Saturday, July 23, 2011
Alice in Intensiveland
This following is excerpted from "Alice in Intensiveland. Being an Essay on Nonsense and Common Sense in the ICU, After the Manner of Lewis Carrol!" by Robert H. Bartlett, MD, FCCP in CHEST 1995; 108:1129-39. I recently read this article, which is a really amusing and impressive allegory of Alice the Medical Student contributing to ICU care by applying her basic knowledge of physiology.
"Being a medical student, Alice perceived the hospital as a place of wonder. Being a medical student, Alice thought of herself (if she ever thought of herself) as intelligent, practical, educable, compassionate, and potentially competent to care for the sick. All she needed to accomplish this task was knowledge, and armed with 2 years worth ofbasic facts, she now sought to acquire that knowledge in this Wonderful Place. She had, metaphorically of course, consumed and deleted, grown and shrunk, read the lines and between the lines, and passed through her own reflection to get here. Now she was ready to begin the grand adventure. That was when she saw Dr. Rabbit.
Dr. Rabbit was hurrying down the hallway, walking so briskly and looking so nervously at his watch that he nearly knocked her over. White shoes, white pants, white tunic covered by a white coat stained by some unidentified biologic fluid. Dr. Rabbit was an intern, but he looked like a White Knight of the Wonderful Place to Alice."
The story then describes Alice confronting the ICU team about treatment of shock, ventilator settings, and other problems for which we occasionally blindly treat without thinking of the physiology. This story features this poem (about how the radical is blamed for things it shouldn't be):
"Jabberwoxy
T'was septic and the slimy rods
Did gyre and gimble in the blood.
All mimsy were the neutrophobs
More air to fuel the flaming flood.
Gramneggars sting and conflagrate
The neutrophobs perfuse acquire
Good oxygas to generate
a Jabberwox to feed the fire.
With vorpal sword well catalyzed
by iron and selenium
Jabberwox killed bugs despised
and mayhaps endothelium.
Dilemma lacking common sense
A preconcepted man could make
On Jabberwoxy evidence
A categorical mistake.
So good or bad it has become
A scientific fadical
For most of academicum
To ridicule the radical.
Twas septic and the slimy rods
Did gyre and gimble in the blood.
All mimsy were the neutrophobs
More air to fuel the flaming flood."
"Being a medical student, Alice perceived the hospital as a place of wonder. Being a medical student, Alice thought of herself (if she ever thought of herself) as intelligent, practical, educable, compassionate, and potentially competent to care for the sick. All she needed to accomplish this task was knowledge, and armed with 2 years worth ofbasic facts, she now sought to acquire that knowledge in this Wonderful Place. She had, metaphorically of course, consumed and deleted, grown and shrunk, read the lines and between the lines, and passed through her own reflection to get here. Now she was ready to begin the grand adventure. That was when she saw Dr. Rabbit.
Dr. Rabbit was hurrying down the hallway, walking so briskly and looking so nervously at his watch that he nearly knocked her over. White shoes, white pants, white tunic covered by a white coat stained by some unidentified biologic fluid. Dr. Rabbit was an intern, but he looked like a White Knight of the Wonderful Place to Alice."
The story then describes Alice confronting the ICU team about treatment of shock, ventilator settings, and other problems for which we occasionally blindly treat without thinking of the physiology. This story features this poem (about how the radical is blamed for things it shouldn't be):
"Jabberwoxy
T'was septic and the slimy rods
Did gyre and gimble in the blood.
All mimsy were the neutrophobs
More air to fuel the flaming flood.
Gramneggars sting and conflagrate
The neutrophobs perfuse acquire
Good oxygas to generate
a Jabberwox to feed the fire.
With vorpal sword well catalyzed
by iron and selenium
Jabberwox killed bugs despised
and mayhaps endothelium.
Dilemma lacking common sense
A preconcepted man could make
On Jabberwoxy evidence
A categorical mistake.
So good or bad it has become
A scientific fadical
For most of academicum
To ridicule the radical.
Twas septic and the slimy rods
Did gyre and gimble in the blood.
All mimsy were the neutrophobs
More air to fuel the flaming flood."
Wednesday, July 20, 2011
Where Are All the Pages?
Interns get paged a lot. Last year, I easily got 20-30 pages a day, from nurses, consultants, medical students ("where are you?"), administration, and friends. Other interns (like surgical colleagues) get even more pages, and it's insane. If you imagine it takes 2-3 minutes to return a page (in an ideal world), that's an hour spent on the phone. We learn to dread our pagers and to celebrate when we forward our pagers and leave the hospital. Even hearing someone else's pager vibrate or ring triggers a reflexive touch to the hip.
That all changed this year. Moving from being an intern to a second-year resident and switching programs to anesthesia (where we aren't primary teams for patients and where everyone knows where to find us) is mindboggling. I get a page a day, or less, and often the page I get each day is myself testing out my pager (is it working? No one's tried to contact me for hours!). No more interruptions, more efficient work, and less scut. It's awesome.
That all changed this year. Moving from being an intern to a second-year resident and switching programs to anesthesia (where we aren't primary teams for patients and where everyone knows where to find us) is mindboggling. I get a page a day, or less, and often the page I get each day is myself testing out my pager (is it working? No one's tried to contact me for hours!). No more interruptions, more efficient work, and less scut. It's awesome.
Tuesday, July 19, 2011
The IV
 One of the most basic medical procedures is the placement of the intravenous line. Nearly everyone who comes into the emergency department, hospital, or operating room gets an IV for administration of medications and blood tests. Every nurse and medical student learns how to start one. But doctors don't do it often. In fact, I didn't start any IVs last year as a medicine intern. In an institution like Stanford with plentiful ancillary services, physicians simply don't need to put in IVs. We only get contacted when several nurses have tried and failed. And in that case, there's no way I would get one when practitioners far better have tried.
One of the most basic medical procedures is the placement of the intravenous line. Nearly everyone who comes into the emergency department, hospital, or operating room gets an IV for administration of medications and blood tests. Every nurse and medical student learns how to start one. But doctors don't do it often. In fact, I didn't start any IVs last year as a medicine intern. In an institution like Stanford with plentiful ancillary services, physicians simply don't need to put in IVs. We only get contacted when several nurses have tried and failed. And in that case, there's no way I would get one when practitioners far better have tried.But then I started anesthesiology. Anesthesiologists are the physicians who probably put in the most IVs since we're responsible for them for every operation. Indeed, we are often the last resort when no one else can get an IV. My first week, I had more failed IVs than successful ones. I was really grateful for my patients' and attendings' patience. But after practice and watching more experienced practitioners, the process clicked. Today, I managed to start a couple difficult IVs on my first try, including one on a patient over 350lbs and an elderly woman with transparent paper-thin skin. It felt good. IVs can be one of the most frustrating and yet satisfying procedures even though it is one of the most basic things health care practitioners do.
Image is in the public domain.
Monday, July 18, 2011
HIV
I haven't seen as much HIV/AIDS at Stanford as I had during medical school in San Francisco. This is simply a reflection of the differences in patient populations. The city was one of the first places to be swept by HIV, and the practitioners there gravitated toward the disease. As a medical student, I worked with some physicians who saw the phenomenon in its infancy, before we understood the disease or what it meant. Hearing their stories was really inspirational. These heroes of medicine reached out to those who were young and sick and dying in droves. No one knew how the disease was spread. No one knew how to treat it. But some of the doctors at UCSF were the first to describe the natural history of the disease and care for its victims. It was wonderful to learn from some of the pioneers of the disease. I saw a dozen patients on my medicine rotation at San Francisco General Hospital including a case of acute HIV (I blogged about this a long time ago).
It surprised me the other day to realize that so far in residency I've only had a handful of patients with HIV/AIDS. I'm okay with this. I chose Stanford knowing that its patient population differs so much from that of San Francisco. But this was also another reminder of the importance of broadening my training environments and clinical experiences to see as much as I can.
It surprised me the other day to realize that so far in residency I've only had a handful of patients with HIV/AIDS. I'm okay with this. I chose Stanford knowing that its patient population differs so much from that of San Francisco. But this was also another reminder of the importance of broadening my training environments and clinical experiences to see as much as I can.
Saturday, July 16, 2011
Lines
Setting up a room might not seem like a big deal, but it's one of the jobs of the anesthesiologist. Operating rooms can get crowded really quickly, and in an emergency, knowing where everything is, how everything works, and which lines, tubes, and cords are critical matter. One of the initially overwhelming things starting out is the number of things between the patient and the machines - mainting airway and IV access, measuring blood pressure, temperature, carbon dioxide, EKG, and oxygen, providing electricity to different gadgets, draining urine and stomach fluid, etc. In my first few days, all of these got tangled up and I couldn't figure out which lines did what. Only with time have I started to learn to organize all these tubes and cords to protect the patient (for example, the airway should be on top so that other cords do not drag it down and pull the breathing tube out). For any entrepreneurs, I wonder if cordless or wireless devices could someday be implemented to cut down on the clutter in the operating room. In any case, I think it's interesting to write about the small things because someday I'll look back and realize all of this has become second nature.
Friday, July 15, 2011
Stand Back! I'm Going to Try Science!
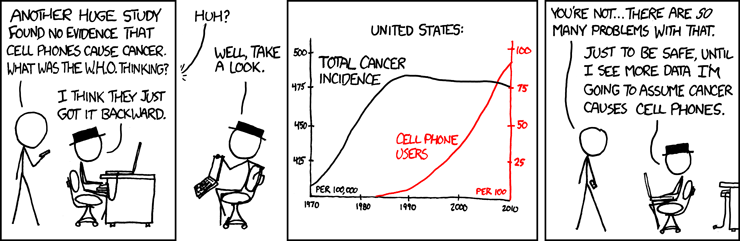 Image is from xkcd, drawn by Randall Munroe, shown under Creative Commons Attribution License.
Image is from xkcd, drawn by Randall Munroe, shown under Creative Commons Attribution License.
Thursday, July 14, 2011
Drugs
Part of the early learning in anesthesia is familiarizing myself with perioperative medications. Many of these are new - etomidate, succinylcholine, neostigmine - and a few are ones I've used before - phenylephrine, fentanyl, midazolam. But learning a dozen new medications is one of the challenges of starting a new specialty. Furthermore, many anesthetics are dosed based on ideal body weight, and so getting a feel of the right dose for each patient also takes times (it took me all of intern year to start estimating successfully doses of vancomycin and piperacillin/tazobactam for patients based on their age, weight, and renal function). No matter how much we like pharmacology (and all applicants applying to anesthesia say they like pharmacology), learning the drugs is hard. Not only that, we are responsible for knowing the pharmacokinetics, pharmacodynamics, duration, interactions, indications, and side effects for these medications. How do we choose between them? What do we see when they are administered?
Even more than that, we have to give the medications ourselves. Medicine was one step removed; I would write an order and expect the medication to be administered. Now, I push the drugs into the IV. So some of my learning is acquiring the manual dexterity to draw up drugs quickly, memorizing the concentration of each drug, and learning to dilute drugs. It helps me remember not to take for granted the time needed to prepare and give medications.
Even more than that, we have to give the medications ourselves. Medicine was one step removed; I would write an order and expect the medication to be administered. Now, I push the drugs into the IV. So some of my learning is acquiring the manual dexterity to draw up drugs quickly, memorizing the concentration of each drug, and learning to dilute drugs. It helps me remember not to take for granted the time needed to prepare and give medications.
Tuesday, July 12, 2011
Overwhelming
Beginnings are hard, and anesthesia is no different. As I move from the cerebral explore-all-possibilities in drawn-out-rounds of medicine to the fast-paced hurry of the operating room, I can feel myself become more and more stressed. There is always time pressure in the operating room. I've found that optimizing efficiency is all about preparation of details. Before the start of the case, I rip small pieces of tape with little tabs for easy access, lined up neatly along the edge of a workspace like elementary school. I pre-label syringes, arrange my monitors, and line up medications in the order they are needed.
Despite preparation, I still find anesthesia chaotic. I'll write more in depth later about the process of inducing anesthesia and placing a breathing tube into a patient, but it can get overwhelming very fast. It requires substantial multitasking and yet significant concentration on one job. There's so much sensory input to filter - seeing the vocal cords, the patient's breathing, the misting on the mask, the arrangement of my tools; hearing the monitor's beeps (both routine and alarm), the cycling of the blood pressure cuff, the sound of the bellows on the ventilator; feeling the squeeze of the bag as a proxy for lung compliance, the fit of the mask to exclude an air leak, the position of the head, the pressure on the teeth. At first, I can only process these things sequentially and I rely on my attending to interpret things faster and anticipate problems.
I think the two central lessons I learned in my first week of anesthesia is to prepare for everything, and then to learn what I didn't prepare for and anticipate it next time. It's a stressful and overwhelming environment, but I'm sure I will adapt to it soon.
Despite preparation, I still find anesthesia chaotic. I'll write more in depth later about the process of inducing anesthesia and placing a breathing tube into a patient, but it can get overwhelming very fast. It requires substantial multitasking and yet significant concentration on one job. There's so much sensory input to filter - seeing the vocal cords, the patient's breathing, the misting on the mask, the arrangement of my tools; hearing the monitor's beeps (both routine and alarm), the cycling of the blood pressure cuff, the sound of the bellows on the ventilator; feeling the squeeze of the bag as a proxy for lung compliance, the fit of the mask to exclude an air leak, the position of the head, the pressure on the teeth. At first, I can only process these things sequentially and I rely on my attending to interpret things faster and anticipate problems.
I think the two central lessons I learned in my first week of anesthesia is to prepare for everything, and then to learn what I didn't prepare for and anticipate it next time. It's a stressful and overwhelming environment, but I'm sure I will adapt to it soon.
Monday, July 11, 2011
A New Start
Sunday, July 10, 2011
First Day
On my first day of anesthesia, I showed up a little before 6, changed into scrubs, and found my operating room. Indeed, I was the first to get there; the medication cabinet was locked, the lights were off, the room was silent. I took the machine through my first machine check, oriented myself to my workspace, drew up the drugs I would need, set out emergency medications. I made several trips back and forth from the anesthesia workroom and figured out how to get my narcotics from the secure dispensing machine. The patients then arrived in holding and I struggled a little to put in an IV just as my attending arrived.
The first case was a repair of a finger fracture. The regional anesthesia team placed a brachial plexus block for us. The case was straightforward, and I spent the time learning my bearings, figuring out how to chart, and familiarizing myself with the flow of the operation.
The second case likewise was a simple toe amputation done under local anesthesia and light sedation. However, there were some concerns because the patient was actively using cocaine which can be lethal if we had to convert to general anesthesia. The surgeons determined that the amputation was somewhat emergent and we proceeded without difficulty. Two easy cases under monitored anesthesia care, and I was feeling good about this. It's not too bad, I thought to myself.
My last case of the day was an add-on of an emergent airway, which sobered me up quickly. A gentleman had come into the emergency department with a large neck mass and difficulty breathing. He had a progressively enlarging thyroid that was beginning to compress his trachea (windpipe) so that he couldn't lie flat to sleep. On exam, even without a stethoscope, I could hear the narrowing of his airway when he breathed, called stridor. This was going to be a difficult case. The surgeons wanted to remove the thyroid, but in order to do so, we'd have to secure a way of ventilating him and helping him breathe. The standard fashion of placing a breathing tube involves lying them flat and inducing general anesthesia, but in this case, we would have no guarantee that if we sedated him and paralyzed him that we'd be able to get into the trachea. We'd have to do this awake.
We anesthetized the back of the patient's throat with nebulized (aerosolized) lidocaine; this is the most important part of the preparation as gag and cough reflexes are incredibly powerful and trying to place a breathing tube in an awake patient can be very uncomfortable and technically difficult if adequate local anesthesia is not provided. Then, I went in with a fiberoptic flexible bronchoscope - a thin camera - and identified the vocal cords and passed the scope into the trachea. I slid an endotracheal tube over the scope into the airway. It was quite exciting as this is one of the more advanced airway techniques, and I had a lot of support from two attendings. The case was also complicated as the patient was persistently hypotensive and required a phenylephrine drip, but luckily we got through it without difficulty. The day ended at 6pm when we had a debriefing with my other co-residents. What a first day!
The first case was a repair of a finger fracture. The regional anesthesia team placed a brachial plexus block for us. The case was straightforward, and I spent the time learning my bearings, figuring out how to chart, and familiarizing myself with the flow of the operation.
The second case likewise was a simple toe amputation done under local anesthesia and light sedation. However, there were some concerns because the patient was actively using cocaine which can be lethal if we had to convert to general anesthesia. The surgeons determined that the amputation was somewhat emergent and we proceeded without difficulty. Two easy cases under monitored anesthesia care, and I was feeling good about this. It's not too bad, I thought to myself.
My last case of the day was an add-on of an emergent airway, which sobered me up quickly. A gentleman had come into the emergency department with a large neck mass and difficulty breathing. He had a progressively enlarging thyroid that was beginning to compress his trachea (windpipe) so that he couldn't lie flat to sleep. On exam, even without a stethoscope, I could hear the narrowing of his airway when he breathed, called stridor. This was going to be a difficult case. The surgeons wanted to remove the thyroid, but in order to do so, we'd have to secure a way of ventilating him and helping him breathe. The standard fashion of placing a breathing tube involves lying them flat and inducing general anesthesia, but in this case, we would have no guarantee that if we sedated him and paralyzed him that we'd be able to get into the trachea. We'd have to do this awake.
We anesthetized the back of the patient's throat with nebulized (aerosolized) lidocaine; this is the most important part of the preparation as gag and cough reflexes are incredibly powerful and trying to place a breathing tube in an awake patient can be very uncomfortable and technically difficult if adequate local anesthesia is not provided. Then, I went in with a fiberoptic flexible bronchoscope - a thin camera - and identified the vocal cords and passed the scope into the trachea. I slid an endotracheal tube over the scope into the airway. It was quite exciting as this is one of the more advanced airway techniques, and I had a lot of support from two attendings. The case was also complicated as the patient was persistently hypotensive and required a phenylephrine drip, but luckily we got through it without difficulty. The day ended at 6pm when we had a debriefing with my other co-residents. What a first day!
Friday, July 08, 2011
Machines
 A lot of beginning anesthesia residency is understanding the machine, and it's a little overwhelming at first. This is in contrast to medicine where I did not have to learn any complex tools (the ultrasound is as far as I got). Anesthesia machines remind me of computers. They are incredibly powerful, automated, and complex. Different companies make different models, and we have to be facile in going from one machine to another. There are lots of connections, plugs, mechanical switches, and buttons. The interface isn't entirely intuitive, but seems like something I'll figure out as I start playing with it. A massive amount of information is generated, and our job is to interpret all of that to keep the patient safe. Today, we learned to do the machine check - to run through a daily algorithm that tests every failsafe and critical aspect of the ventilator, gas delivery systems, monitors, and connections. It's a little daunting as we are expected to troubleshoot any problems or malfunction of the machine all while keeping the patient safe. But I like technology, and so I think picking this up will come pretty quickly.
A lot of beginning anesthesia residency is understanding the machine, and it's a little overwhelming at first. This is in contrast to medicine where I did not have to learn any complex tools (the ultrasound is as far as I got). Anesthesia machines remind me of computers. They are incredibly powerful, automated, and complex. Different companies make different models, and we have to be facile in going from one machine to another. There are lots of connections, plugs, mechanical switches, and buttons. The interface isn't entirely intuitive, but seems like something I'll figure out as I start playing with it. A massive amount of information is generated, and our job is to interpret all of that to keep the patient safe. Today, we learned to do the machine check - to run through a daily algorithm that tests every failsafe and critical aspect of the ventilator, gas delivery systems, monitors, and connections. It's a little daunting as we are expected to troubleshoot any problems or malfunction of the machine all while keeping the patient safe. But I like technology, and so I think picking this up will come pretty quickly. Image of Datex Ohmeda anesthesia machine is in the public domain, from Wikipedia.
Wednesday, July 06, 2011
Reorientation
The first few days of "anesthesia" actually consist of a lot of orientation. We see many new faces and departments - human resources, pharmacy, medical records, security & compliance, billing. We get whirlwind tours of the operating rooms, meet future attendings and senior residents, and learn the logistics at each hospital. For me, this is a small breather because I'm familiar with the basics from internship. Although it's a slow start, at least I feel fairly low stress and can share some tips and tricks. I await the end of the week when we actually start clinical responsibilities.
Tuesday, July 05, 2011
Book Review: Final Exam
 I recently read Pauline Chen's Final Exam, a narrative nonfiction on a surgeon's perspective on death and dying. It's interesting; many of the sentiments, experiences, and thoughts expressed in the book are reflected in my blogs over the last five years. The surgical approach, however, is fascinating. She speaks of issues specific to surgeons - the idea of performing an operation on someone who subsequently dies, the infamous morbidity and mortality conferences, the surgical culture.
I recently read Pauline Chen's Final Exam, a narrative nonfiction on a surgeon's perspective on death and dying. It's interesting; many of the sentiments, experiences, and thoughts expressed in the book are reflected in my blogs over the last five years. The surgical approach, however, is fascinating. She speaks of issues specific to surgeons - the idea of performing an operation on someone who subsequently dies, the infamous morbidity and mortality conferences, the surgical culture.The writing in the book is excellent; it's clear, articulate, eloquent, graceful. The chapters read almost like essays with interwoven patient narratives and stories. To be honest, reading it felt like re-experiencing that which I'd already seen, so I don't think I particularly learned or gained much. It might not be the right book for a resident or physician. But I think it's a great read for the pre-med or interested layperson. The literature on death and dying perseverates on the disconnect between physicians and their familiarity, comfort, and understanding of the end of life. But what I'm trying to find goes beyond that - I know what it's like to care for a dying person, but my question is how we can change the system, structure, people, education, or expectations to make it better.
Image shown under Fair Use, from paulinechen.typepad.com
Monday, July 04, 2011
Farewell to Internal Medicine
It feels odd that the last year, I worked so hard to learn as much of internal medicine as I could, and now I'm changing fields. I really immersed myself in medicine, especially since it was a close second in career choice. I love it, and it seems core to what I've enjoyed in the last five years. I feel that I could have easily become a second year medicine resident. I will miss it. Medicine encompasses a lot of what I imagined when I thought of being a doctor prior to medical school, and I have a certain affinity to it. There are people who never liked the endless rounding, the theory and pathophysiology, the thinking but not doing - but I was never one of those people.
Now that I am starting a new and exciting field, I'm sure I'll keep my medicine tools handy; I'll continue to follow along peripherally and learn some of the cutting-edge developments. I'll read consultations closely because I enjoy it, I'll keep my experiences in the last year close to my heart. I'm sure I'll run into my colleagues in the hospital. Some say anesthesia is simply medicine of the operating room, and I hope that my internship will serve me well.
Now that I am starting a new and exciting field, I'm sure I'll keep my medicine tools handy; I'll continue to follow along peripherally and learn some of the cutting-edge developments. I'll read consultations closely because I enjoy it, I'll keep my experiences in the last year close to my heart. I'm sure I'll run into my colleagues in the hospital. Some say anesthesia is simply medicine of the operating room, and I hope that my internship will serve me well.
Saturday, July 02, 2011
1300
 This is the pale blue dot, Earth as seen from Voyager 1 at the edge of the solar system, 3,762,136,324 miles from home.
This is the pale blue dot, Earth as seen from Voyager 1 at the edge of the solar system, 3,762,136,324 miles from home."Look again at that dot. That’s here. That’s home. That’s us. On it everyone you love, everyone you know, everyone you ever heard of, every human being who ever was, lived out their lives. The aggregate of our joy and suffering, thousands of confident religions, ideologies, and economic doctrines, every hunter and forager, every hero and coward, every creator and destroyer of civilization, every king and peasant, every young couple in love, every mother and father, hopeful child, inventor and explorer, every teacher of morals, every corrupt politician, every ‘superstar,’ every ‘supreme leader,’ every saint and sinner in the history of our species lived there - on a mote of dust suspended in a sunbeam.
The Earth is a very small stage in a vast cosmic arena. Think of the rivers of blood spilled by all those generals and emperors so that, in glory and triumph, they could become the momentary masters of a fraction of a dot. Think of the endless cruelties visited by the inhabitants of one corner of this pixel on the scarcely distinguishable inhabitants of some other corner, how frequent their misunderstandings, how eager they are to kill one another, how fervent their hatreds.
Our posturings, our imagined self-importance, the delusion that we have some privileged position in the Universe, are challenged by this point of pale light. Our planet is a lonely speck in the great enveloping cosmic dark. In our obscurity, in all this vastness, there is no hint that help will come from elsewhere to save us from ourselves.
The Earth is the only world known so far to harbor life. There is nowhere else, at least in the near future, to which our species could migrate. Visit, yes. Settle, not yet. Like it or not, for the moment the Earth is where we make our stand.
It has been said that astronomy is a humbling and character-building experience. There is perhaps no better demonstration of the folly of human conceits than this distant image of our tiny world. To me, it underscores our responsibility to deal more kindly with one another, and to preserve and cherish the pale blue dot, the only home we’ve ever known." - Carl Sagan.
Image shown under Fair Use, from Tecnoscience.
Friday, July 01, 2011
July 1st
It amazes me that medicine is a field where every year on a prescribed day, the entire workforce of academic hospitals across the nation turns over. As I've mentioned in the past, for reasons I don't fully appreciate, July 1st is the day when new housestaff begin. Newly graduated medical students become interns; weary interns become residents; graduating residents become attendings or fellows. The entire hierarchy moves up a level on the same day. What other industry would dare do that? How could this tradition be sustained for decades? We all laugh timidly when we joke "July 1st is the most dangerous day to go to a hospital" but how true is this statement? Are we really doing those we serve a disservice by standardizing the day when everyone steps into new shoes and takes new roles?
This transition is not to be underestimated. Housestaff - interns, residents, fellows - essentially run the hospital. We make the gears turn. So on July 1st, a whole new cohort of faces must learn those hard skills that the outgoing interns spent a whole year learning. Even ignoring the aspect of medical knowledge, I remember trying to figure out how to get from ward to ward, send pages, put in orders, discharge patients. Of course, we all support each other, and the new residents remember vividly when (just yesterday) they were interns. So it all works out. Sort of.
I am sure there are benefits to this system, that somehow it's the way things must work with the academic year of graduating medical students, the importance starting a whole cohort together, the coordination between different hospitals that swap residents. July 1st may be here to stay, so I wish you best of health this month.
This transition is not to be underestimated. Housestaff - interns, residents, fellows - essentially run the hospital. We make the gears turn. So on July 1st, a whole new cohort of faces must learn those hard skills that the outgoing interns spent a whole year learning. Even ignoring the aspect of medical knowledge, I remember trying to figure out how to get from ward to ward, send pages, put in orders, discharge patients. Of course, we all support each other, and the new residents remember vividly when (just yesterday) they were interns. So it all works out. Sort of.
I am sure there are benefits to this system, that somehow it's the way things must work with the academic year of graduating medical students, the importance starting a whole cohort together, the coordination between different hospitals that swap residents. July 1st may be here to stay, so I wish you best of health this month.
Subscribe to:
Comments (Atom)



