How do you approach a family to say that medical care is futile and ought to be stopped? How do you look at a patient on cardiovascular drips, a mechanical ventilator, artificial nutrition, continuous renal replacement therapy, and broad-spectrum antibiotics and decide to stop them? Even if a patient will never get better, they are alive now, and what does it mean to stop those interventions keeping them alive? Modern medical ethics makes a point to say that withdrawing support is ethically equivalent to not beginning the support in the first place. Had we known this patient was not a transplant candidate and would not get better, we would not have intubated her, started pressors, continued CVVH. But now that we have started these things, it's so much harder to stop them, even if nominally there's no difference.
I spend two hours in family meetings over two days. End of life conversations are never easy. But over time, I've become better. I make a point to plan things out. I find a quiet room. I introduce everyone, learn everyone's names. I ask family what their understanding of the situation is. I explain the medical issues as clearly as I can; I avoid vagaries. I survey responses, from "I cannot stand her suffering; I think we should let her go in peace" to "I'm not God, I don't know what to do" to "I don't understand, why is this happening" to "I need more time" to "I think a miracle might still happen." When asked, I make my medical recommendation, that futile care should not be prolonged, that the patient is suffering, and that we should move to comfort care once everyone who needs to be here has arrived. With each meeting, I inch toward that goal. Although medically, we can unilaterally transition the patient to comfort care, my job now is to care for the family and help them cope.
Sunday, September 30, 2012
Saturday, September 29, 2012
Futility I
Medical futility refers to an intervention that has no expectation to help at all. It is often raised in circumstances near the end of life when families push for treatments that physicians feel are futile. Ethically, a treatment does not have to be rendered - even if requested by a patient or family member - if it is futile. As a silly example, if a patient asked me for antibiotics for migraine treatment, I could decline simply because it is futile. Since it has no benefit, there is no circumstance in which the benefits outweigh the risks. This becomes infinitely more complex in the case of a terminal illness. In someone with end-stage cancer, how do you know that antibiotics won't help? Or herbal treatments? Or surgery? But if a physician feels these are futile, they need not be entertained.
A patient is admitted with fulminant liver failure; she is confused from hepatic encephalopathy, has gained 20 pounds, has massive fluid in her abdomen, and begins to bleed. No one knows why her liver has failed; she has cryptogenic cirrhosis. Subsequently, she develops hepatorenal syndrome and requires dialysis. During the hospitalization, she has a cardiac arrest requiring chest compressions; she's intubated and placed on a mechanical ventilator. She is admitted to the ICU where I meet her. With tenuous blood pressures, she no longer tolerates hemodialysis and requires CVVH. Unfortunately, because of her medical comorbidities, she is denied a liver and kidney transplant. Despite maximizing all our medical interventions, she does not get better, and now that she cannot get a transplant, we have nothing left to offer. She will die from multiorgan system dysfunction, and though our interventions can stave off that moment, none have the possibility of stopping it. This is, we feel, futile care.
A patient is admitted with fulminant liver failure; she is confused from hepatic encephalopathy, has gained 20 pounds, has massive fluid in her abdomen, and begins to bleed. No one knows why her liver has failed; she has cryptogenic cirrhosis. Subsequently, she develops hepatorenal syndrome and requires dialysis. During the hospitalization, she has a cardiac arrest requiring chest compressions; she's intubated and placed on a mechanical ventilator. She is admitted to the ICU where I meet her. With tenuous blood pressures, she no longer tolerates hemodialysis and requires CVVH. Unfortunately, because of her medical comorbidities, she is denied a liver and kidney transplant. Despite maximizing all our medical interventions, she does not get better, and now that she cannot get a transplant, we have nothing left to offer. She will die from multiorgan system dysfunction, and though our interventions can stave off that moment, none have the possibility of stopping it. This is, we feel, futile care.
Wednesday, September 26, 2012
1600
This is the 1600th post! When I wrote the blog several days ago about pharmaceutical companies, I realized I wanted to comment on ads. I made a decision long ago not to put ads on this blog. At that time, it was sponsored by UCSF and I didn't need or want ads. Over time, I have had several inquiries about placing links, advertisements, or commercial sponsors on this blog and my Case of the Day blog. Although I like the idea of making money, I decided that it was best to keep them pure, unmuddied, and unhindered by outside influences. Now that we're here at post 1600, I'm pretty happy about how everything's turned out.
Tuesday, September 25, 2012
Back in the Medical ICU
I'm back in the unit. It's been a little rough because even though things are easier each time around, I feel like I'm shouldering more responsibility. As an anesthesiologist, I'm used to doing everything myself; since we often work alone, we develop a craving and knack for independence. We are also completely and solely responsible for our patients. We become obsessive about details. As a result, the intensive care unit can be tough for us as we navigate team dynamics and relinquish our micromanaging tendencies. The issue I am finding with the team dynamic of the ICU is that residents come with differing levels of experience, knowledge, strengths, motivations, and standards. Certainly, I have gotten much better as a result of my 4 previous months in the intensive care unit (2 as a medicine intern, 2 as an anesthesia resident). But it means that I feel responsible for every detail for every patient on the service, and that becomes completely exhausting. Although it may be good for patients that I catch things other residents overlook, it's unhealthy for me. I obsess over things that seem small but that I find important - nutrition, lines, prophylaxis, antibiotic regimens, frequency of labs, wound care. Most of the others on the team, especially if it is their first month in the unit, forget these things, and I try my best to catch anything that falls through. In the big picture, this extra work probably doesn't translate to huge gains in care, but I feel obligated to do it nevertheless.
So overall, I have mixed feelings back in the unit. I love the medicine, the procedures, the evidence-based decisions, the complexity, the teaching (both as a student and to students). But it will be a tiring and hard month, and I'm bracing myself to learn to delegate more, obsess less, prioritize better, and take care of myself during this rotation.
So overall, I have mixed feelings back in the unit. I love the medicine, the procedures, the evidence-based decisions, the complexity, the teaching (both as a student and to students). But it will be a tiring and hard month, and I'm bracing myself to learn to delegate more, obsess less, prioritize better, and take care of myself during this rotation.
Monday, September 24, 2012
False Negatives
Old school general surgeons will say that if you don't get false negative appendectomies, then you aren't operating enough. That is to say, the diagnosis of appendicitis is not specific enough for any surgeon to be 100% sure for every single patient whether she has appendicitis or not. If every time he operates, he finds an inflamed appendix, then he is missing the diagnosis in some of those cases in which he thinks there is no appendicitis. Only by overoperating - that is, performing an appendectomy but finding a normal appendix - can he be sure that he has actually gotten all the cases of appendicitis.
In the same way, in the ICU, one could say that if you aren't re-intubating patients, then you aren't aggressive enough in extubating them. I believe this; the duration of intubation has a lot of risks, especially ventilator associated pneumonia. But to be aggressive enough in extubation so that everyone gets a chance at being extubated early, some subset of those patients won't fly and will require re-intubation. This is often seen as a failure, but in truth, if we waited for the tail end of that bell curve, everyone else would have the tube longer than necessary.
I kind of like this thought process (though articulating it is tough). I'm not sure whether it's true or not, but as I progress in residency and get a better sense of risks and benefits, I begin to find this sort of justification compelling.
In the same way, in the ICU, one could say that if you aren't re-intubating patients, then you aren't aggressive enough in extubating them. I believe this; the duration of intubation has a lot of risks, especially ventilator associated pneumonia. But to be aggressive enough in extubation so that everyone gets a chance at being extubated early, some subset of those patients won't fly and will require re-intubation. This is often seen as a failure, but in truth, if we waited for the tail end of that bell curve, everyone else would have the tube longer than necessary.
I kind of like this thought process (though articulating it is tough). I'm not sure whether it's true or not, but as I progress in residency and get a better sense of risks and benefits, I begin to find this sort of justification compelling.
Saturday, September 22, 2012
Pharmaceutical Influences
Meetings of the local chapter of the California Society of Anesthesiologists (CSA) are sponsored by a pharmaceutical company. They take place at a nice restaurant, have a guest physician speaker who talks about a new product on the market, and present an update of political topics by anesthesiology leaders in the CSA.
I attend these. Partly, I feel that it is important to participate in the local community of anesthesiologists, to be aware of the issues, to network, and to get a sense of the broader direction of medicine. In the insulated world of residency, our perspectives and viewpoints are limited. How do big changes in healthcare affect the livelihood of physicians, specifically anesthesiologists? What issues are we advocating for, what are we lobbying for? I also go because admittedly, the dinners are quite good. I don't feel strongly about the talks; I know they are biased and designed to persuade me.
The problem, of course, is that I am influenced by these pharmaceutical companies. I've read some of the data about the subconscious effect of dinner talks and gifts, and I've heard ex-pharmaceutical reps speak about their methods of persuasion. I know that the purist would abstain from these meetings, and so I feel quite morally ambiguous about attending them. I write this to explore, ponder, and verbalize these ethical conundrums.
I attend these. Partly, I feel that it is important to participate in the local community of anesthesiologists, to be aware of the issues, to network, and to get a sense of the broader direction of medicine. In the insulated world of residency, our perspectives and viewpoints are limited. How do big changes in healthcare affect the livelihood of physicians, specifically anesthesiologists? What issues are we advocating for, what are we lobbying for? I also go because admittedly, the dinners are quite good. I don't feel strongly about the talks; I know they are biased and designed to persuade me.
The problem, of course, is that I am influenced by these pharmaceutical companies. I've read some of the data about the subconscious effect of dinner talks and gifts, and I've heard ex-pharmaceutical reps speak about their methods of persuasion. I know that the purist would abstain from these meetings, and so I feel quite morally ambiguous about attending them. I write this to explore, ponder, and verbalize these ethical conundrums.
Friday, September 21, 2012
Perioperative Medicine
Although most people think of an anesthesiologist as the gas-man during surgery, we often fill the role of the perioperative medicine physician to the surgeons before, during, and after surgery. Yesterday, I provided anesthesia for a patient with congenital prolonged QT syndrome and one with severe restrictive lung disease from scoliosis. Of course, these patients had been seen by their cardiologist and pulmonologist prior to surgery, who helped with optimization of medications and acquisition of appropriate tests. However, as the anesthesiologist for these patients, I was the one who had to interpret the data and recommendations. How do we plan an anesthetic that minimizes QT prolongation and reduces risk of arrhythmia? What rescue medications and monitoring is required? I realized that the surgeons didn't have a good grasp of the syndrome when they asked me if the patient could get any opiates. (In our electronic medical record, opiates trigger a warning because methadone prolongs QT and similar drugs alarm the system). For the patient with a precarious pulmonary status, I had to decide whether to extubate the patient, and even if extubated, whether an intensive care bed was more appropriate. I advised the surgeons with regard to medications to avoid, therapies to reduce atelectasis, and pain control techniques to reduce splinting. All this reminded me that even if patients see their specialists, anesthesiologists are often the doctors who remind surgeons how best to address the nonsurgical issues.
Wednesday, September 19, 2012
Resident Well-Being
Resident well-being is one of those topics that most physicians find either very important or extraordinarily dull. Some of the old-timers, those who walked uphill both ways in snow, take the attitude that there was no focus on their well-being and they turned out fine, so why all this hubbub about making sure we're happy? Others, the movers and shakers, are realizing exhausted, unhappy, depressed, and ill residents are not good for patient care, do not create great physicians, and are not an ethical part of training. Residents have a very biased view of things. But overall, Stanford is not a harsh or malignant program and most residents feel like their wellness is valued. Nevertheless, it is interesting when I compare my position to peers in other fields. I work over sixty hours in a hospital, yet I haven't seen my own doctor in ages. I've learned not to take for granted weekends or days off - every day is a work day unless told otherwise. I've been inculcated in a hierarchical structure, one that discourages us from speaking up against our mentors. Stress is a regular, real, and expected part of my job. In small quantities, perhaps these things are reasonable, but a system that seeks to train leaders may have to have different values.
Tuesday, September 18, 2012
ADD
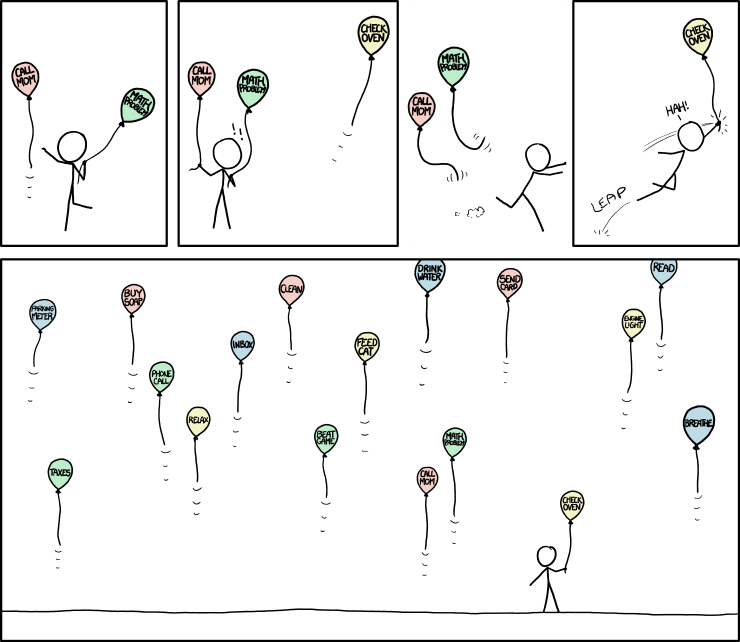
Click to enlarge. I love this xkcd comic because this phenomenon doesn't just apply to those with ADD; I often feel like this as a resident. As I'm handling one thing, I get paged about the previous patient, then I remember I have to prepare the next patient, and suddenly the surgeon is requesting something, alarms begin to beep, and I realize the room is full of balloons. As I progress in anesthesia training, I become better at prioritizing, creating routines for myself, adhering to checklists, and multitasking when necessary.
Image is from xkcd, drawn by Randall Munroe, shown under Creative Commons Attribution License.
Monday, September 17, 2012
Fun
As I finish my two months in pediatric anesthesia, I reflect on how fun days are simply because of our patients. Although adults may be able to think rationally, tolerate discomfort, and communicate with words, they are rarely charming, adorable, or playful. But every day, even if the anesthesia is unremarkable, the children are not. Some kids show an amazing resilience, showing courage as they ask about different things they see in the operating rooms. Some have a huge desire to please and can be coerced with promises of stickers or popsicles. Some kids simply have cute smiles. I shouldn't underestimate the pleasure of working with children, and I will miss doing so when I switch to the ICU next week.
Image of child shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Image of child shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Sunday, September 16, 2012
Challenge
An attending challenged me to come up with two anesthetic plans for the same type of case. So for two ear surgeries, I designed one anesthetic based entirely on intravenous agents and one with inhaled anesthetics. I usually do these cases with one technique, but the attending believed that no technique had an absolute clear advantage in the uncomplicated case, and indeed, the unconventional approach has its own benefits. I was surprised to find this to be true. The ENT surgeon thanked us for using nitrous oxide as it helped his visualization of the middle ear. With careful planning to attenuate the side effects of the volatile anesthetic approach, I found that what I feared - nausea and a slow wake-up - did not happen at all. In fact, I felt that the unconventional anesthetic performed superior to the standard technique.
There are many ways to achieve a successful anesthetic to some surgeries. While everyone at one institution may do it one way, this reminds me that other approaches, if planned, designed, and executed well, can achieve the same or better outcome. There are always ongoing drug shortages and the possibility of equipment failure, and this makes me more comfortable that I can continue treating patients even in the event that my hands are tied by one thing or another.
There are many ways to achieve a successful anesthetic to some surgeries. While everyone at one institution may do it one way, this reminds me that other approaches, if planned, designed, and executed well, can achieve the same or better outcome. There are always ongoing drug shortages and the possibility of equipment failure, and this makes me more comfortable that I can continue treating patients even in the event that my hands are tied by one thing or another.
Wednesday, September 12, 2012
Syndromes
One of the unique aspects of pediatric medicine is that we interact with children with syndromes. Syndromes are often the result of a genetic mutation and can lead to multiorgan involvement. Resultant defects may require surgical repair, and so the anesthesiologist needs to be familiar with common, uncommon, and rare syndromes. Some, like the Pierre-Robin sequence, involve airway abnormalities that can make intubation challenging if not impossible. Many involve cardiac anomalies, and if these are not recognized, patients can be gravely harmed.
Today, I provided anesthesia for a patient with an incredibly rare genetic mutation. In looking it up, I found that only 40-some cases have been described in the literature. It demonstrates the incredible impact a single gene mutation can have; this child had developmental delay, high risk of strokes, an abnormal stature, dysplasia of the bones, an immunocompromised state, and kidney failure. Careful research of the disease in question, meticulous planning, and communication with the multidisciplinary providers were central to providing a safe and appropriate anesthetic.
Today, I provided anesthesia for a patient with an incredibly rare genetic mutation. In looking it up, I found that only 40-some cases have been described in the literature. It demonstrates the incredible impact a single gene mutation can have; this child had developmental delay, high risk of strokes, an abnormal stature, dysplasia of the bones, an immunocompromised state, and kidney failure. Careful research of the disease in question, meticulous planning, and communication with the multidisciplinary providers were central to providing a safe and appropriate anesthetic.
Tuesday, September 11, 2012
Regional Anesthesia
When we're on the adult anesthesia side, there's a dedicated regional anesthesia team to do nerve blocks for appropriate surgeries: knee replacements, elbow surgeries, rotator cuff repairs. But on pediatrics, we get the opportunity to do blocks since there is no separate attending and resident for regional techniques. The challenges are different. Most nerve blocks are done while the patient is awake so that we can evaluate the efficacy of the block and monitor for adverse events. As you can imagine, children don't usually tolerate a needle attached to a nerve stimulator going into their neck. Sedation, distraction (for one teenager, we played a hip hop music video on the OR TVs), preparation, and reassurance are necessary for a smooth block. So far, I've seen and done some upper extremity nerve blocks for elbow and wrist surgeries, and it's been pretty fun.
The most common block, however, is the caudal block, which is placed in infants and toddlers and gives good pain relief for many surgeries below the umbilicus. In the same manner as an epidural, except using a tiny 22g IV catheter, we palpate landmarks on the baby's low back and insert a shallow needle into the epidural space and inject local anesthetic and clonidine. The pain relief is pretty remarkable as patients wake up comfortable after many different general, urologic, and orthopedic surgeries.
The most common block, however, is the caudal block, which is placed in infants and toddlers and gives good pain relief for many surgeries below the umbilicus. In the same manner as an epidural, except using a tiny 22g IV catheter, we palpate landmarks on the baby's low back and insert a shallow needle into the epidural space and inject local anesthetic and clonidine. The pain relief is pretty remarkable as patients wake up comfortable after many different general, urologic, and orthopedic surgeries.
Monday, September 10, 2012
Lifestyle
I was on home call this weekend and only had to go into the hospital once for an emergency appendectomy. In thinking about this, I was reminded that compared to most specialties, anesthesiology is pretty amenable to a nice lifestyle. Unlike other fields with constant inpatient responsibilities, voluminous telephone calls, or clinical workloads spread among few residents, anesthesia is lucky to have more flexibility, pretty reasonable call shifts, and no primary hospital services. But what I like about my colleagues is that few people enter the field solely for its lifestyle. Cases are often punctuated with highly stressful moments and the weekdays can be intense and long. Many other fields are even more benign with few or no emergencies, free weekends, and days that don't start at six. Fields like radiology, dermatology, ophthalmology, pathology have strong draws for those wanting more free time. But I can't deny that anesthesia offers a great work-life balance.
I love anesthesia because it offers a highly technically, medically complex, (occasionally easy) case load with a predictable workweek and usually a weekend reprieve. While I never really shirked from the tough 30 hour intern calls, I do appreciate being able to take advantage of free time and post-call days that aren't consumed by sleep. "Lifestyle specialties" often get a bad rap for "taking the easy way out," and for a while I wondered whether I'd be bothered by it, but now I feel that as long as my job is satisfying and I'm serving patients, I'm happy and guilt-free during my newly discovered abundance of free time.
I love anesthesia because it offers a highly technically, medically complex, (occasionally easy) case load with a predictable workweek and usually a weekend reprieve. While I never really shirked from the tough 30 hour intern calls, I do appreciate being able to take advantage of free time and post-call days that aren't consumed by sleep. "Lifestyle specialties" often get a bad rap for "taking the easy way out," and for a while I wondered whether I'd be bothered by it, but now I feel that as long as my job is satisfying and I'm serving patients, I'm happy and guilt-free during my newly discovered abundance of free time.
Sunday, September 09, 2012
Geological Time Spiral
Click to enlarge. I found this picture and really liked the aesthetic nature of outlining human evolution on a geological time scale. It reminds me how minute and small human beings and human doings are in the history of the Earth. It provides a little perspective that those quite-important things I worry about are quite-important in their own respect, and also quite measured from other viewpoints.
Image is in the public domain, from Wikipedia.
Friday, September 07, 2012
Private Practice
I had a couple of what is often described as "private practice days." In one of them, I had nine surgeries, all ear tubes and/or tonsils and adenoids. On another day, I had radiation therapy, GI procedures, liver biopsies, and bone marrow biopsies. These are pretty common days for the anesthesiologist in an ambulatory surgery center. Most children are pretty healthy, the procedures are minor, and patients go home the day of the surgery. Providing adequate anesthesia isn't hard, but the goal is to optimize the efficiency and flow of the day. Patients, surgeons, and staff don't tolerate slow anesthetics, and even a delay of five minutes per case can easily translate to an hour behind schedule. Likewise, the anesthesiologist cannot let a bottleneck of patients build up in the recovery room, and good pain and nausea control is necessary to get kids home in a timely fashion. So these days actually require a lot of preparation, planning, and efficiency to keep everyone happy.
Wednesday, September 05, 2012
Simulation and Consent
I wanted to blog briefly on two very separate topics, simulation and consent in pediatrics. We have a few educational simulations in pediatric anesthesia to play out rare situations such as cardiac arrest or local anesthetic toxicity. The way these simulations are done is interesting because we keep repeating the same scenario over and over again (with each resident playing a different role). The purpose is for us to assimilate the algorithms of treatment into our muscle memory so that if the rare situation arises, we won't be completely off guard. At first, I wasn't sure this was the best way of using simulation - after all, wouldn't it be more educational to do lots of different cases? But after doing the same thing over and over, the actions ("Resume chest compressions, give 10mcg/mg epinephrine IV, what are the possible H's and T's?") become boring because we're so familiar with them, and that's what you want in an emergency.
On a completely different note, being in pediatrics reminds me how complex consent can be. For adult procedures, consent is (fairly) simple; for the most part, patients can understand what to expect with anesthesia and decide whether to have it. But for kids, surrogate decision makers have to determine the best course of action. What do you do when a child refuses something the parents want (pretty much any surgery for a toddler)? What if it's a teenager? What do you do if one parent desires something that the other declines? Is a phone consent as good as an in-person consent (and is the fact that the parent isn't present for their child's surgery an indication of anything?). There are the legal black-and-white answers and then there are practical ones. For example, one child undergoes a procedure requiring blood transfusions and his father is a Jehovah's witness - how do we approach that situation? Legally, we can (and should) transfuse if medically indicated, but how do we broach the topic with the parents? There are many nuances I'm learning as I work with kids.
On a completely different note, being in pediatrics reminds me how complex consent can be. For adult procedures, consent is (fairly) simple; for the most part, patients can understand what to expect with anesthesia and decide whether to have it. But for kids, surrogate decision makers have to determine the best course of action. What do you do when a child refuses something the parents want (pretty much any surgery for a toddler)? What if it's a teenager? What do you do if one parent desires something that the other declines? Is a phone consent as good as an in-person consent (and is the fact that the parent isn't present for their child's surgery an indication of anything?). There are the legal black-and-white answers and then there are practical ones. For example, one child undergoes a procedure requiring blood transfusions and his father is a Jehovah's witness - how do we approach that situation? Legally, we can (and should) transfuse if medically indicated, but how do we broach the topic with the parents? There are many nuances I'm learning as I work with kids.
Tuesday, September 04, 2012
Sick Kids
Unfortunately, any physician working with children will encounter sick patients. I forgot this aspect of pediatrics. So when providing anesthesia to children for radiation therapy, the hardest part was the emotional realization that these children had cancer, and often cancer that was incurable. Even when I get "exciting" anesthesia cases such as a craniotomy for a posterior fossa tumor, it means that a child has a brain cancer. This is hard. And even though anesthesia providers are consultants - we don't have to deliver the news, talk to the parents, follow the child through chemotherapy - we still feel that emotional tear, the irrational feeling that some things in this world are not fair. These children and their families who battle illnesses I cannot even fathom, they are incredibly strong, incredibly brave.
Sunday, September 02, 2012
Radiation Therapy
One of the black boxes of medicine, even to doctors, is radiation oncology. Physicians know more or less what all their colleagues do, except for the elusive radiation oncologists. We send our cancer patients to get radiation without knowing exactly what it entails. For the first time, I saw external beam radiation rooms and machines as I had to provide anesthesia to children for treatments. Although the therapy is not painful, it requires the patient to stay quite still while a loud machine whirls about them. Teenagers and adults can tolerate the treatment, but children often need general anesthesia for the five or ten minutes while the cancer is zapped. It's not difficult since the patients all have indwelling vascular access ports for their chemotherapy. But it is an interesting environment because it is so remote. After inducing anesthesia, we leave the room and monitor the patient with video cameras while the room is irradiated. Because treatments recur daily for weeks, patients get very resistant to propofol and require sky-high doses. Conversely though, the anesthesia is easy because we simply repeat what worked in the past. Overall, it is a different facet of anesthesia for me to learn, and it was interesting to see the inner workings of one aspect of radiation oncology.
Image shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Image shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Saturday, September 01, 2012
Blue Moon
Last night, I noticed the most brilliant moon and realized it was the second full moon of the month. Time seems to pass quicker and quicker. All of a sudden, August is over, supermarkets are stocked with Halloween candy, and pediatric anesthesia slows down as kids go back to school. In a few months, I will have to decide what I want to do for fellowship - post-resident training. In a year and a half, I should be a fully qualified independent anesthesiologist. There never seems to be time to rest, time to coast, time to slack. I am a little envious of my friends in other jobs who have achieved a peaceful routine, who aren't always racing toward the next checkpoint, in constant acceleration. Most of the time, I don't mind it; after all, this is the path I've traced out for myself, with its unique satisfactions and humbling responsibilities.
Blue Moon from yesterday, taken in Ecuador, shown under Creative Commons Attribution Share-Alike License, from Wikipedia.
Subscribe to:
Comments (Atom)