Extremely unpolished, but fresh in my head.
-
Day One: ICU on Call
Feet hurt, coat heavy
pockets sag, pens strewn
checkboxes and papers folded
in all manners of origami.
I sit to write and
an alarm goes off; a beeping pager;
a call with new labs; a family;
a nurse tapping my shoulder
casting thoughts
across the water.
Blue drape, ultrasound shadows
gloves of a second skin
and a needle the size of a pen.
Surprised I don't tremble,
afraid forehead droplets
might fall onto the field.
Headache means something new now.
Fishing weights thrust upon my eyelids
a ball and chain I heft
as I run to room five.
A vet asks me to cut his hair.
He is joking. I don't get it.
As long as I'm standing
I won't fall over. I lean
on the portable computers
and shift weight from side to side
wiggle my toes
hide a yawn behind the monitor.
Someone sick comes in.
It's like I'd just woken up.
I have palpitations. I should sit
but instead I rush in
before noticing
contact precaution signs.
I avoid the nurse's glare.
You can tell which ones are gonna make it
and which ones won't almost on arrival,
but the sadness doesn't hit
until I'm the cot, forgetting I still have my shoes on.
I kick them off, then cry
thinking of a man who walked into the hospital
and will never walk out
but before I wipe my face I'm gone.
Cradle in the fetal position
one hand clasping a pager
the other around a cell phone
like an infant's rattle.
Halfway through the twenty minutes
I'm cold, but I don't have time
to reach down and pull up the blanket.
The screech of the pager goes off
and I fumble for my shoes; why'd I
kick them off anyway? Out the darkness
squinting my way down the hall
stethoscope like a squid around my neck.
You'd think more people would quit by now
but that thought never enters my head.
Tuesday, June 29, 2010
Monday, June 28, 2010
Looking Forward
My very last day at UCSF was capstoned with an hour of reflection. Some of the great teachers and clinicians gave us heartfelt inspirational talks about graduation, becoming a doctor, and entering residency. Some spoke about the deep meaning of their work every day, and their passion was contagious. I could hear in the voice of one of the homeless clinic preceptors the importance of taking care of those with very little. I remembered the importance of teaching as I listened to an instructor's excitement about seeing a new class each year. I laughed at the humor of a neurologist who asked us to balance levity with reflection. But the most substantive exercise, surprisingly enough, was touchy-feely. One of the great Brain, Mind, Behavior professors asked us to meditate, and we did. Meditation is often hard because it requires some suspension of disbelief; for those of us who meditate infrequently, it feels like a sham. We're just closing our eyes. Our mind is wandering to lunch. But he guided us with a soft and reassuring voice; we were moved. We thanked everyone who helped us through medical school, we wished them well. We thanked those we didn't get along with, and also wished them well. Collectively, I felt something special as we ruminated on the people in our lives, and not only those most important to us, but those who are nameless and would otherwise have been forgotten. I don't think we do enough reflection, and it was wonderfully refreshing to do so.
Friday, June 25, 2010
Setting Sail
"To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all" - Sir William Osler.
Today is my first day really being a doctor. Residency begins today, and I am starting as an intern in the VA intensive care unit. It's fascinating to hear how intern year is described. Those who just went through it can't believe they survived. Those a few years out still shudder with the thought. Those who are far out and gray-haired talk about it as the best year of their life. We, just about to enter it, do so with a morbid curiosity and great trepidation. This is our first test as a physician, and it's no longer multiple choice. We will learn, we will grow, we will cry, we will rejoice, we will suffer. It is time to widen the range of ability, emotion, compassion, self-confidence, and possibility.
I feel nervous, meek, somewhat an imposter, somewhat a charlatan. My white coat does not fit me. But I am here, and I am expected. It is not by accident that I'm a doctor. I can do this. What are my goals for this very first day? Get to know some patients. Don't make any egregious errors. Eat something. Don't break down. Start simple, right?
Today is my first day really being a doctor. Residency begins today, and I am starting as an intern in the VA intensive care unit. It's fascinating to hear how intern year is described. Those who just went through it can't believe they survived. Those a few years out still shudder with the thought. Those who are far out and gray-haired talk about it as the best year of their life. We, just about to enter it, do so with a morbid curiosity and great trepidation. This is our first test as a physician, and it's no longer multiple choice. We will learn, we will grow, we will cry, we will rejoice, we will suffer. It is time to widen the range of ability, emotion, compassion, self-confidence, and possibility.
I feel nervous, meek, somewhat an imposter, somewhat a charlatan. My white coat does not fit me. But I am here, and I am expected. It is not by accident that I'm a doctor. I can do this. What are my goals for this very first day? Get to know some patients. Don't make any egregious errors. Eat something. Don't break down. Start simple, right?
Thursday, June 24, 2010
Some Fine Print
I have been debating what to do with this blog now that I'm starting residency. I will of course keep writing, and I decided to do so here rather than in a separate blog or a private journal. Asclepion has been my record of medical training and residency is simply a continuation of that. However, the time pressures of residency will compress my blogs and rein in my gregariousness; the frequency of writing will change but I'll try to keep a diversity of posts. I still have a few topics lingering from medical school I'd like to write about, so those will come at the beginning of next week before I start writing about orientation and my first rotation.
This is still a personal website with sometimes-whimsical musings; its purpose is merely a journal of reflection for myself and nothing more than that. Here's the fine print: though I am a doctor, this blog does not provide any medical advice, and information here should not be construed as such. Reading and using this website does not create a physician-patient relationship and is not intended to replace the services of a licensed, trained physician or health care professional. No health or medical related decision should be based in whole or in part on anything contained here. Any opinions expressed here are not necessarily mine nor do they reflect the opinions of any of my affiliations. Content on this site may be changed without notice and is not guaranteed to be complete, correct, or up-to-date. I reserve the right to edit or delete comments posted to this site.
This is still a personal website with sometimes-whimsical musings; its purpose is merely a journal of reflection for myself and nothing more than that. Here's the fine print: though I am a doctor, this blog does not provide any medical advice, and information here should not be construed as such. Reading and using this website does not create a physician-patient relationship and is not intended to replace the services of a licensed, trained physician or health care professional. No health or medical related decision should be based in whole or in part on anything contained here. Any opinions expressed here are not necessarily mine nor do they reflect the opinions of any of my affiliations. Content on this site may be changed without notice and is not guaranteed to be complete, correct, or up-to-date. I reserve the right to edit or delete comments posted to this site.
Wednesday, June 23, 2010
How Does a Hospital Work?
One of the interesting and very sad realities is that despite being a physician, I know very little about how a hospital works. We got one lecture on this at the end of medical school, and that's probably more than most. Learning about the hospital is very much part of the "hidden curriculum" and acculturation of working at one. Many things confuse me; for example, how come nurses are hired by the hospital or medical center whereas doctors (medical staff) are not? Why is the CEO usually not an MD? How do costs and revenues work? Is the hospital paid by procedure or by diagnosis? What about a clinic? Do labs and radiology count as inpatient or outpatient services (surprisingly, I have a hunch that for billing, they're more similar to outpatient services). Who's the chief operational officer or the chief medical officer or the chief of staff, and what do they do? So much happens in the background, behind the eyes of patient and provider. I couldn't tell you the order of magnitude of hospital expenses or where they go (non-MD personnel? equipment? capital improvements? overhead?). I couldn't tell you how many operators we have or how many people working on insurance claims.
Then there are the nuts and bolts of regulation: what does it mean to be credentialed? What could cause my hospital (or residency program) to lose accreditation? What happens if we think a fellow physician shouldn't be practicing? Now that we're becoming more and more aware of patient safety, I'm learning about infection control and quality improvement. But I'm still not sure what they check: perioperative beta blockers? ICU glycemic control? acute MI responses? codes? other things?
Most medical students know about the Joint Commission because when they inspect the hospital, we need to be on our best behavior. But what about CMS (Centers for Medicare and Medicaid services) or the Leapfrog group or this business with "centers of excellence"? We all have fuzzy notions of what is tracked (time to antibiotic for pneumonia, readmission rates for CHF, surgical site infections, resident work hours) but we never formally get taught these things. As we switch from rotation to rotation, we learn to use two patient identifiers for a time-out, expect read-back with verbal orders, and look for checklists. But what are the repercussions of failing to adhere to standards? If my publicly reported hospital performance is marred, how does that affect my day-to-day life? Or the hospital's viability? What about the new-fangled physician ratings websites that allow you to look up specific providers? How does that work?
I think this is interesting. The culture of safety will be a great boon to patients and to the delivery of care. But because it's so new, there's little formal instruction. Likewise, we don't need to know hospital finances but what if one day we want to become an administrator ourselves? This sort of thing isn't in the curriculum and is lower priority than the knowledge base to take care of patients, but we don't want to omit it completely.
Then there are the nuts and bolts of regulation: what does it mean to be credentialed? What could cause my hospital (or residency program) to lose accreditation? What happens if we think a fellow physician shouldn't be practicing? Now that we're becoming more and more aware of patient safety, I'm learning about infection control and quality improvement. But I'm still not sure what they check: perioperative beta blockers? ICU glycemic control? acute MI responses? codes? other things?
Most medical students know about the Joint Commission because when they inspect the hospital, we need to be on our best behavior. But what about CMS (Centers for Medicare and Medicaid services) or the Leapfrog group or this business with "centers of excellence"? We all have fuzzy notions of what is tracked (time to antibiotic for pneumonia, readmission rates for CHF, surgical site infections, resident work hours) but we never formally get taught these things. As we switch from rotation to rotation, we learn to use two patient identifiers for a time-out, expect read-back with verbal orders, and look for checklists. But what are the repercussions of failing to adhere to standards? If my publicly reported hospital performance is marred, how does that affect my day-to-day life? Or the hospital's viability? What about the new-fangled physician ratings websites that allow you to look up specific providers? How does that work?
I think this is interesting. The culture of safety will be a great boon to patients and to the delivery of care. But because it's so new, there's little formal instruction. Likewise, we don't need to know hospital finances but what if one day we want to become an administrator ourselves? This sort of thing isn't in the curriculum and is lower priority than the knowledge base to take care of patients, but we don't want to omit it completely.
Tuesday, June 22, 2010
Cross Cover and Sign Out
Although most people view the "difficult" stuff in medicine as making that astute diagnosis, responding to emergencies, and finessing treatment plans, the most dangerous part of next year for me will be navigating a process called sign out. In sign out, one physician transfers the information and responsibility for care of a patient to another physician. This occurs a lot. At the end of each day, teams sign out their patients to the on-call doctors. At some point in the evening, a night resident (called a "float") comes in and receives sign-out from the on-call team. While most patients have no issues at night, if something does happen, the doctor who responds won't be the doctor who knows them best. This is a necessary part of the system; otherwise, all residents would be at the hospital all the time. Furthermore, sign outs are becoming more prevalent because of work-hour restrictions. Residents aren't allowed to be at the hospital for more than 30 hours at a time (or 80 hours in a week) so at the end of a 30-hour shift, someone else must take responsibility for the care of the patients. (Cross-cover, which is in the title of the post is a similar sort of situation).
Interestingly, I got a talk about sign-out from UCSF at the end of our last block "Coda" and a talk from Stanford during our orientation; this is how important that process is. It's compounded by so many more difficulties; outgoing residents are exhausted and want to go home, on-call residents are swamped with work; patients are extraordinarily complicated. Most medical students have seen the "there's nothing to do on my patients" sign-out and that's simply not adequate, though it's tempting. Communication is central to so many preventable errors. Thus, it was great to get two recent lectures on this process (and good to know that the key points were the same at both places) and hopefully I will keep this in mind as I start later this week.
Interestingly, I got a talk about sign-out from UCSF at the end of our last block "Coda" and a talk from Stanford during our orientation; this is how important that process is. It's compounded by so many more difficulties; outgoing residents are exhausted and want to go home, on-call residents are swamped with work; patients are extraordinarily complicated. Most medical students have seen the "there's nothing to do on my patients" sign-out and that's simply not adequate, though it's tempting. Communication is central to so many preventable errors. Thus, it was great to get two recent lectures on this process (and good to know that the key points were the same at both places) and hopefully I will keep this in mind as I start later this week.
Sunday, June 20, 2010
Poem: The Velluvial Matrix
The Velluvial Matrix
gossamer threads descending
streamers and occasion extending
inverted grass of silver and light
sticky with the weight and stare
of a thousand velluvia, tall
and gray, eyes like judgment
and bound by your conscience
this velluvial matrix shimmers
with impermanence and honesty
this is what you've chosen
to peer into the darkest mines
and pitch a tent alongside mystery
grasped and pulled all directions
this cage of imagination
leaves you free as can be
gossamer threads descending
streamers and occasion extending
inverted grass of silver and light
sticky with the weight and stare
of a thousand velluvia, tall
and gray, eyes like judgment
and bound by your conscience
this velluvial matrix shimmers
with impermanence and honesty
this is what you've chosen
to peer into the darkest mines
and pitch a tent alongside mystery
grasped and pulled all directions
this cage of imagination
leaves you free as can be
Saturday, June 19, 2010
The Velluvial Matrix
Atul Gawande gave the commencement speech for the Stanford School of Medicine and I really enjoyed reading it.
"Half a century ago, medicine was neither costly nor effective. Since then, however, science has combatted our ignorance. It has enumerated and identified, according to the international disease-classification system, more than 13,600 diagnoses—13,600 different ways our bodies can fail. And for each one we’ve discovered beneficial remedies—remedies that can reduce suffering, extend lives, and sometimes stop a disease altogether. But those remedies now include more than six thousand drugs and four thousand medical and surgical procedures. Our job in medicine is to make sure that all of this capability is deployed, town by town, in the right way at the right time, without harm or waste of resources, for every person alive. And we’re struggling. There is no industry in the world with 13,600 different service lines to deliver.
It should be no wonder that you have not mastered the understanding of them all. No one ever will. That’s why we as doctors and scientists have become ever more finely specialized. If I can’t handle 13,600 diagnoses, well, maybe there are fifty that I can handle—or just one that I might focus on in my research. The result, however, is that we find ourselves to be specialists, worried almost exclusively about our particular niche, and not the larger question of whether we as a group are making the whole system of care better for people. I think we were fooled by penicillin. When penicillin was discovered, in 1929, it suggested that treatment of disease could be simple—an injection that could miraculously cure a breathtaking range of infectious diseases. Maybe there’d be an injection for cancer and another one for heart disease. It made us believe that discovery was the only hard part. Execution would be easy.
But this could not be further from the truth. Diagnosis and treatment of most conditions require complex steps and considerations, and often multiple people and technologies. The result is that more than forty per cent of patients with common conditions like coronary artery disease, stroke, or asthma receive incomplete or inappropriate care in our communities. And the country is also struggling mightily with the costs. By the end of the decade, at the present rate of cost growth, the price of a family insurance plan will rise to $27,000. Health care will go from ten per cent to seventeen per cent of labor costs for business, and workers’ wages will have to fall. State budgets will have to double to maintain current health programs. And then there is the frightening federal debt we will face. By 2025, we will owe more money than our economy produces. One side says war spending is the problem, the other says it’s the economic bailout plan. But take both away and you’ve made almost no difference. Our deficit problem—far and away—is the soaring and seemingly unstoppable cost of health care."
I definitely think it was important and timely for Dr. Gawande to raise these issues, especially to a graduating class of physicians entering the health care system at this time. What can we do to confront these problems? How can we create and maintain a sustainable political and economic framework for healthcare? How can we adapt to the overwhelming and impossible complexity of science and medicine?
The excerpt is from The New Yorker; entire speech can be found here:
http://www.newyorker.com/online/blogs/newsdesk/2010/06/gawande-stanford-speech.html
"Half a century ago, medicine was neither costly nor effective. Since then, however, science has combatted our ignorance. It has enumerated and identified, according to the international disease-classification system, more than 13,600 diagnoses—13,600 different ways our bodies can fail. And for each one we’ve discovered beneficial remedies—remedies that can reduce suffering, extend lives, and sometimes stop a disease altogether. But those remedies now include more than six thousand drugs and four thousand medical and surgical procedures. Our job in medicine is to make sure that all of this capability is deployed, town by town, in the right way at the right time, without harm or waste of resources, for every person alive. And we’re struggling. There is no industry in the world with 13,600 different service lines to deliver.
It should be no wonder that you have not mastered the understanding of them all. No one ever will. That’s why we as doctors and scientists have become ever more finely specialized. If I can’t handle 13,600 diagnoses, well, maybe there are fifty that I can handle—or just one that I might focus on in my research. The result, however, is that we find ourselves to be specialists, worried almost exclusively about our particular niche, and not the larger question of whether we as a group are making the whole system of care better for people. I think we were fooled by penicillin. When penicillin was discovered, in 1929, it suggested that treatment of disease could be simple—an injection that could miraculously cure a breathtaking range of infectious diseases. Maybe there’d be an injection for cancer and another one for heart disease. It made us believe that discovery was the only hard part. Execution would be easy.
But this could not be further from the truth. Diagnosis and treatment of most conditions require complex steps and considerations, and often multiple people and technologies. The result is that more than forty per cent of patients with common conditions like coronary artery disease, stroke, or asthma receive incomplete or inappropriate care in our communities. And the country is also struggling mightily with the costs. By the end of the decade, at the present rate of cost growth, the price of a family insurance plan will rise to $27,000. Health care will go from ten per cent to seventeen per cent of labor costs for business, and workers’ wages will have to fall. State budgets will have to double to maintain current health programs. And then there is the frightening federal debt we will face. By 2025, we will owe more money than our economy produces. One side says war spending is the problem, the other says it’s the economic bailout plan. But take both away and you’ve made almost no difference. Our deficit problem—far and away—is the soaring and seemingly unstoppable cost of health care."
I definitely think it was important and timely for Dr. Gawande to raise these issues, especially to a graduating class of physicians entering the health care system at this time. What can we do to confront these problems? How can we create and maintain a sustainable political and economic framework for healthcare? How can we adapt to the overwhelming and impossible complexity of science and medicine?
The excerpt is from The New Yorker; entire speech can be found here:
http://www.newyorker.com/online/blogs/newsdesk/2010/06/gawande-stanford-speech.html
Friday, June 18, 2010
Revision: Galileo, Galileo
Galileo, Galileo
Hope you never get this page:
Your patient jumped out the window.
They are resuscitating him downstairs.
Downstairs, sidewalk flecked with gum
shining with mica
blood like thrown art
where a man learns
clouds are less dense
and sidewalks denser than flesh.
In fifth grade, we made homes for five story eggs.
We made omelets on the sidewalk.
I had just spoken with him.
He combed his beard
and asked for an apple.
I didn't tell the nurse.
Galileo, Galileo.
He tossed the chair
then became the chaser.
The roommate paints
arms spread eagle,
hair in ropes ascending
hospital gown parachute.
Why didn't you stop him?
I wonder.
Wish I noticed something,
wish he mentioned voices
wish a first floor bed was open
wish I could sleep at night.
How could it be
like fate like gravity
nothing suffices
leaving apology and guilt wanting.
You wrestle my pager from me,
tell me to go home.
Galileo, Galileo.
Good night.
Hope you never get this page:
Your patient jumped out the window.
They are resuscitating him downstairs.
Downstairs, sidewalk flecked with gum
shining with mica
blood like thrown art
where a man learns
clouds are less dense
and sidewalks denser than flesh.
In fifth grade, we made homes for five story eggs.
We made omelets on the sidewalk.
I had just spoken with him.
He combed his beard
and asked for an apple.
I didn't tell the nurse.
Galileo, Galileo.
He tossed the chair
then became the chaser.
The roommate paints
arms spread eagle,
hair in ropes ascending
hospital gown parachute.
Why didn't you stop him?
I wonder.
Wish I noticed something,
wish he mentioned voices
wish a first floor bed was open
wish I could sleep at night.
How could it be
like fate like gravity
nothing suffices
leaving apology and guilt wanting.
You wrestle my pager from me,
tell me to go home.
Galileo, Galileo.
Good night.
Thursday, June 17, 2010
Revision: Mythology, and Other Lies
Mythology, and Other Lies
The Greeks knew then the liver’s secret,
that with succor of ambrosia and nectar,
it defies absolution. By liver, I mean both
organ and organism as Prometheus
pulled off a trick thirty thousand years ago
that we haven’t figured out yet,
regenerating both himself and that purveyor of iron.
We’ve only deciphered the latter
and named it transplant, a term that conjures
the idea of sexually ineffable bryophytes
and ferns and fern-allies.
And yet, I am not so sure we aren’t Titans,
that we aren’t chained to some precipice
to have our organs devoured
leaving the hull of our drive empty.
Every day, I renew that gourd and drink deep
to brace myself for vultures I know must come
yet whose presence I continue to doubt.
The Greeks knew then the liver’s secret,
that with succor of ambrosia and nectar,
it defies absolution. By liver, I mean both
organ and organism as Prometheus
pulled off a trick thirty thousand years ago
that we haven’t figured out yet,
regenerating both himself and that purveyor of iron.
We’ve only deciphered the latter
and named it transplant, a term that conjures
the idea of sexually ineffable bryophytes
and ferns and fern-allies.
And yet, I am not so sure we aren’t Titans,
that we aren’t chained to some precipice
to have our organs devoured
leaving the hull of our drive empty.
Every day, I renew that gourd and drink deep
to brace myself for vultures I know must come
yet whose presence I continue to doubt.
Wednesday, June 16, 2010
Poem: Wedding
Wedding
Sprawled on clouds, we lay on backs
wearing pajamas, staying past our bedtime
while our counterparts act out a script
in lilac and champagne. They make toasts,
stamp glasses, hoist chairs above heads,
but we, the shadows, play cards at a sixth grade
slumber party, wrestle barefoot in backyard.
Here, bride and I trade stories, we gossip,
we laugh, we remember the time when...
and in the synagogue, she places a ring,
recites Hebrew, creates a time when...
When we begin dancing, the two
come closer--the band blasting karaoke
coaxes us from perches of memory
to throw up our hands and belt along,
loosen those ties, abandon formality
and if you look closely you can see,
we haven't grown up and we don't want to, either.
Sprawled on clouds, we lay on backs
wearing pajamas, staying past our bedtime
while our counterparts act out a script
in lilac and champagne. They make toasts,
stamp glasses, hoist chairs above heads,
but we, the shadows, play cards at a sixth grade
slumber party, wrestle barefoot in backyard.
Here, bride and I trade stories, we gossip,
we laugh, we remember the time when...
and in the synagogue, she places a ring,
recites Hebrew, creates a time when...
When we begin dancing, the two
come closer--the band blasting karaoke
coaxes us from perches of memory
to throw up our hands and belt along,
loosen those ties, abandon formality
and if you look closely you can see,
we haven't grown up and we don't want to, either.
Tuesday, June 15, 2010
Poem: Commencement
Commencement
So, this is what it feels like
he says, hands on the podium,
beginning a speech no one remembers.
I marinate in my own thoughts
wondering, for example, how to scratch
that itch on my back
without knocking over my mortarboard.
People applaud, and I admire
the ceiling of floating acrylic
bending and scattering light
on its way out of the symphony hall.
What if, I wonder, he mentions my name
and I neglect to respond
caught up in smoothing a creased corner
of the program? Wonder is not care.
I feel less present than balconies
of families cheering, and for a person
who stayed up late reflecting
I had little to say to myself.
How does it feel to reach that peak
of Everest, look around, and realize
everyone else there just accomplished
the same thing? To snap
a photograph as if the culmination
could represent the thing itself
like a lake spelling waterfall.
And yet here, I did not want to give this up,
did not want to abandon my wanderlust
because if this is the reward
for hard work, I'll take it.
I spy gallantly robed deans
resting their eyes.
He makes a joke, and perhaps people laugh.
I think of my first day on the job
the first patient who died
the first to unexpectedly live
the nights when I ached for forty minutes of sleep
and the days longing for forty minutes of work.
He lasts about that long
an investment of time
for me to call myself doctor
and yet, I don't really care to get those minutes back.
So, this is what it feels like
he says, hands on the podium,
beginning a speech no one remembers.
I marinate in my own thoughts
wondering, for example, how to scratch
that itch on my back
without knocking over my mortarboard.
People applaud, and I admire
the ceiling of floating acrylic
bending and scattering light
on its way out of the symphony hall.
What if, I wonder, he mentions my name
and I neglect to respond
caught up in smoothing a creased corner
of the program? Wonder is not care.
I feel less present than balconies
of families cheering, and for a person
who stayed up late reflecting
I had little to say to myself.
How does it feel to reach that peak
of Everest, look around, and realize
everyone else there just accomplished
the same thing? To snap
a photograph as if the culmination
could represent the thing itself
like a lake spelling waterfall.
And yet here, I did not want to give this up,
did not want to abandon my wanderlust
because if this is the reward
for hard work, I'll take it.
I spy gallantly robed deans
resting their eyes.
He makes a joke, and perhaps people laugh.
I think of my first day on the job
the first patient who died
the first to unexpectedly live
the nights when I ached for forty minutes of sleep
and the days longing for forty minutes of work.
He lasts about that long
an investment of time
for me to call myself doctor
and yet, I don't really care to get those minutes back.
Sunday, June 13, 2010
Poetry Week
I've been somewhat remiss in writing poems. As Vienna Teng says, "It's been too long, I know. Silence has compound interest. My habit is to declare bankruptcy every few months and hope for clemency." This will be a week of poems, both new and old. If poetry is not your thing, feel free to take a week's vacation and come back next Sunday.
Today's poem is really rough, mostly because it's based on an idea and I'm not sure a poem is the best way to get at it.
-
Hooding
We each invited two to hood us on stage
and I learned the most about my classmates that moment.
Who strode up with confidence to shake the dean's hand,
leaving their parents in their wake?
Whose parents wore traditional garb
and waved to all of Nigeria in the wings?
Who was accompanied by a brother or sister
and why was my mind probing the cause?
Some mothers walked with a limp.
Some fathers led by seeing-eye dogs.
Some graduates hooded by their children.
Some holding babies in their arms.
Some wore resplendent pants beneath gown;
others - perhaps - wore nothing.
From the clicking of heels, you could estimate
how quickly or slowly each graduate ascended
and perhaps how many additional inches
their shoes afforded.
How did I approach the stage, I wonder.
Carried by applause and tremor,
I paid no heed to how I walked
or where I looked, letting instinct
dictate the cadence of my steps.
Today's poem is really rough, mostly because it's based on an idea and I'm not sure a poem is the best way to get at it.
-
Hooding
We each invited two to hood us on stage
and I learned the most about my classmates that moment.
Who strode up with confidence to shake the dean's hand,
leaving their parents in their wake?
Whose parents wore traditional garb
and waved to all of Nigeria in the wings?
Who was accompanied by a brother or sister
and why was my mind probing the cause?
Some mothers walked with a limp.
Some fathers led by seeing-eye dogs.
Some graduates hooded by their children.
Some holding babies in their arms.
Some wore resplendent pants beneath gown;
others - perhaps - wore nothing.
From the clicking of heels, you could estimate
how quickly or slowly each graduate ascended
and perhaps how many additional inches
their shoes afforded.
How did I approach the stage, I wonder.
Carried by applause and tremor,
I paid no heed to how I walked
or where I looked, letting instinct
dictate the cadence of my steps.
Friday, June 11, 2010
The Gold Headed Cane
 The gold headed cane has long been a symbol in medicine. The original cane was carried by John Radcliffe (1652-1714) and passed down from physician to physician through the hands of Richard Mead, Anthony Askew, William Pitcairn, and Matthew Baillie. Each physician, at the end of his career, would identify a colleague of worth and bequeath the cane to him. Back then, the cane was the symbol of the physician much as the white coat is today. With a head of gold, silver, or ivory, the canes were hollow and perforated. Doctors would fill the inside with powders thought to prevent disease. On rounds, as they entered patient rooms, physicians would bang the canes on the ground to aerosolize the compounds. The favorite preparation was "vinegar of the four thieves" or Marseilles vinegar; the story is that four thieves who robbed a plague-stricken Marseilles confessed that they took this aromatic vinegar to prevent catching the contagion. What an odd tradition.
The gold headed cane has long been a symbol in medicine. The original cane was carried by John Radcliffe (1652-1714) and passed down from physician to physician through the hands of Richard Mead, Anthony Askew, William Pitcairn, and Matthew Baillie. Each physician, at the end of his career, would identify a colleague of worth and bequeath the cane to him. Back then, the cane was the symbol of the physician much as the white coat is today. With a head of gold, silver, or ivory, the canes were hollow and perforated. Doctors would fill the inside with powders thought to prevent disease. On rounds, as they entered patient rooms, physicians would bang the canes on the ground to aerosolize the compounds. The favorite preparation was "vinegar of the four thieves" or Marseilles vinegar; the story is that four thieves who robbed a plague-stricken Marseilles confessed that they took this aromatic vinegar to prevent catching the contagion. What an odd tradition.Image of the gold headed cane in the Royal College of Physicians, London shown under Fair Use, from www.rcplondon.ac.uk.
Thursday, June 10, 2010
Review of Systems
Coda also reviewed key concepts in a number of fields. We got the best lecturers to come and speak to us one last time on topics from dermatology to emergency department complaints to intern-year neurology. The neurology session was especially fun because our beloved teachers acted out patient and intern interactions as we reviewed the approach to headache, stroke, weakness, and altered mental status. We revisited topics I still find confusing like acute renal failure, how to approach the geriatric patient, and transfusion medicine. As a medical student, I never needed to know the details of the risks of blood transfusion; next year, I'll be expected to get informed consent for such things. It was also my last chance to learn about something "for fun" in a field I'm not going into; I learned about obstetrical and gynecologic emergencies as well as transplant medicine from the department chair of surgery.
Starting in two weeks, I'll be learning primarily adult internal medicine. While that field is certainly vast, overwhelming, and intimidating enough, I realized from Coda that I've really been introduced to a lot in the last four years. We've looked at every organ system, every stage of life, every major specialty and many smaller ones as well. We started with dissecting a cadaver and progressed to assisting with surgeries in the operating room. We've learned the names and functions of dozens of genes and proteins, forgotten them, replaced that space with names of obscure diseases, and then subsequently forgotten about those as well. A lot of information has passed through my head. Hopefully some of it has stuck. But medical school is as undifferentiated as I will ever be; I learned things all doctors ought to know but which I will use very little in the future. What a weird feeling.
Starting in two weeks, I'll be learning primarily adult internal medicine. While that field is certainly vast, overwhelming, and intimidating enough, I realized from Coda that I've really been introduced to a lot in the last four years. We've looked at every organ system, every stage of life, every major specialty and many smaller ones as well. We started with dissecting a cadaver and progressed to assisting with surgeries in the operating room. We've learned the names and functions of dozens of genes and proteins, forgotten them, replaced that space with names of obscure diseases, and then subsequently forgotten about those as well. A lot of information has passed through my head. Hopefully some of it has stuck. But medical school is as undifferentiated as I will ever be; I learned things all doctors ought to know but which I will use very little in the future. What a weird feeling.
Wednesday, June 09, 2010
Loans
Medical students are terrified of many things. Looking ahead, I'm anxious and nervous about the prospect of internship, being responsible for patients, teaching medical students, long hours, and unanticipated challenges. But even outside the hospital, we face terrifying pressures. Nearly all of us have loans from the last eight years of school, and now they're starting to come into play. Even worse, most of us have no financial sense at all (which is why we went to medical school) and know nothing about managing personal finances.
UCSF graduates have an average of $98,388 in Stafford subsidized loans at 6.8% and some Grad plus loans at 8.5%. To help us navigate the complexity of money, we had a speaker come educate us about personal finances. The problem is that students think differently than "adults." We loathe spending money we find unnecessary; we go to noon conferences for the free food, we identify free museum days. These things of course, are great habits, but as we get older, certain things change. Students are reluctant to get insurance because we think we're invincible and that risk management is an unnecessary expense. But we have to realize that our education, the last eight years, is a huge investment on our part and that we should protect it. Luckily, many residency programs provide medical, dental, disability, and life insurance. But in thinking on this topic, it's an interesting attitude I've noted among young people, especially those without dependents.
Finally, we're starting to make money next year. In the past eight years, prudent loan management dictates that we borrow only what we need. Now with a salary, we will have discretionary income. Do we save the money? Do we invest? Do we go somewhere extravagant on the two weeks of vacation we have? Do we buy a house? Do we pay down our loans? The speaker even delved into Roth IRAs, Deductible 403(b)s, stocks, and bonds. Or should we invest in real estate, private equity, commodities, or hedge funds? All these questions open up a Pandora's box of possibility for graduating medical students. I don't know! I've never learned any of this stuff before.
UCSF graduates have an average of $98,388 in Stafford subsidized loans at 6.8% and some Grad plus loans at 8.5%. To help us navigate the complexity of money, we had a speaker come educate us about personal finances. The problem is that students think differently than "adults." We loathe spending money we find unnecessary; we go to noon conferences for the free food, we identify free museum days. These things of course, are great habits, but as we get older, certain things change. Students are reluctant to get insurance because we think we're invincible and that risk management is an unnecessary expense. But we have to realize that our education, the last eight years, is a huge investment on our part and that we should protect it. Luckily, many residency programs provide medical, dental, disability, and life insurance. But in thinking on this topic, it's an interesting attitude I've noted among young people, especially those without dependents.
Finally, we're starting to make money next year. In the past eight years, prudent loan management dictates that we borrow only what we need. Now with a salary, we will have discretionary income. Do we save the money? Do we invest? Do we go somewhere extravagant on the two weeks of vacation we have? Do we buy a house? Do we pay down our loans? The speaker even delved into Roth IRAs, Deductible 403(b)s, stocks, and bonds. Or should we invest in real estate, private equity, commodities, or hedge funds? All these questions open up a Pandora's box of possibility for graduating medical students. I don't know! I've never learned any of this stuff before.
Tuesday, June 08, 2010
Paper Party
Two of my friends Stephanie and Paul held a "paper party" during Coda. What is a paper party, you might ask. Well, my co-blogger Steph imagined an intellectual exchange of seminal publications between medical school graduates. We all know the residents who can quote studies and attendings who have file cabinets full of papers. So this paper party was supposed to stimulate discussion and accumulation of articles. Steph and Paul lured us in with wine and food, only stipulating that we each bring a study to discuss. Of course, the hodgepodge of papers that arrived were hardly academic. While some of us looked at landmark articles on the use of pulmonary artery catheters, the window for tissue plasminogen activator, and dexamethasone prior to antibiotics for meningitis, there was also a flurry of the weird, inappropriate, and hilarious. Some of the stranger papers included a case study of whether knuckle-cracking leads to arthritis, digital rectal massage for intractable hiccups (and possibly supraventricular tachycardia), and a systematic review of randomized controlled studies on the use of parachutes in falls (my favorite article; BMJ 2003;327;1459-1461). In any case, when people start throwing paper parties, you know we have too much time on our hands.
Sunday, June 06, 2010
Mystery Case

 I have a mystery case! The two images above are of my arm. When I first noticed the lesion, it already looked like the first image. I couldn't recall anything that might have caused it, and I couldn't think of any trauma involving my arm. It appeared all of a sudden. It was not painful or pruritic. The area of central clearing was slightly raised. With strong pressure, it was mildly tender. It didn't feel warmer than surrounding skin. I didn't have any other symptoms. I didn't really know what to make of it, but we concluded it was probably some sort of trauma I couldn't recall.
I have a mystery case! The two images above are of my arm. When I first noticed the lesion, it already looked like the first image. I couldn't recall anything that might have caused it, and I couldn't think of any trauma involving my arm. It appeared all of a sudden. It was not painful or pruritic. The area of central clearing was slightly raised. With strong pressure, it was mildly tender. It didn't feel warmer than surrounding skin. I didn't have any other symptoms. I didn't really know what to make of it, but we concluded it was probably some sort of trauma I couldn't recall.But then two days later, it worsened into the ecchymosis seen in the second image. The area of central clearing was still raised and slightly hard, perhaps a nodule; it was still minimally tender and non-pruritic. Any ideas?
We concluded it might have been some sort of insect bite. It eventually got better and completely cleared within a week, but I figured it was interesting enough for me to take pictures and perhaps someone will come up with a diagnosis. Also, if you like this sort of thing, I do have a separate website: http://caseoftheday.blogspot.com/ with mystery medical cases.
Both images are by me.
Friday, June 04, 2010
Volunteers
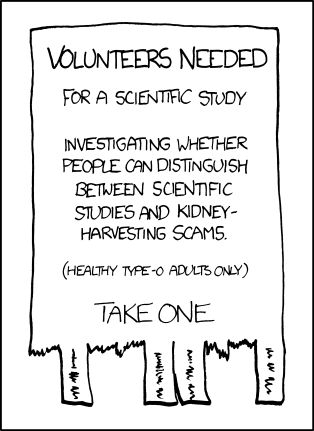 Image from xkcd.com, drawn by Randall Munroe, shown under Creative Commons Attribution-NonCommercial 2.5 License.
Image from xkcd.com, drawn by Randall Munroe, shown under Creative Commons Attribution-NonCommercial 2.5 License.
Thursday, June 03, 2010
Convocation
We had Convocation on Cinco de Mayo. I looked up convocation on Wikipedia (the source on everything eclectic) and learned that it was simply a formal assembly (or a collective noun for eagles). Convocation took place where we began medical school, in Cole Hall, festively decorated with balloons of jalapenos and sombreros. A slideshow depicting key moments in medical school reminded us of so many milestones: the camping trip, orientation, the white coat ceremony, volunteering, electives, parties, fundraisers, cultural shows, vacations, conferences. There was a "virtual parade of children," pictures of all the kids my classmates had and raised during medical school. This is truly a stunning accomplishment; I think of how busy I was and I can't imagine the additional responsibility of caring for a young child. We also presented teaching awards to residents and faculty. I feel that recognizing great teachers is so important but often overlooked. I aspire to be like the residents and faculty who we acknowledged. Lastly, "superlatives" were given to our classmates such as "most likely to be at an event with free food," "most likely to complete 5 residencies," "most likely to have a career in politics," "best shoulder to cry on," and "most likely to oversleep on the first day of residency." It was a really fun celebration with all my classmates.
Wednesday, June 02, 2010
Professional Liability
One of the undertaught but scary things about becoming a "real" doctor is professional liability. What are the legal and ethical issues that come up as I become a resident next year? We got a talk from risk management about the basics of medical malpractice, how insurance works, and common reasons for lawsuits. I always found it interesting that poor communication is a better predictor than actual negligence of whether a lawsuit is brought forth. Of course, poor communication is often core to the problem such as failure to follow-up on abnormal results or improper informed consent. We also reviewed how to disclose an unanticipated adverse event to a patient. How do you tell someone that "something went wrong," and how do you do it if you think you are not at fault or if you are at fault? Such discussions are so difficult to approach and yet every detail is important to determining how things go. I think as I move forward, I am becoming more aware of the legal ramifications of what I do. Statistically, at some point, I will have to go through the process, but hopefully being aware, knowledgeable, and careful will help me avoid any sticky situations.
Tuesday, June 01, 2010
Learning in Coda
The difficulty with structuring a curriculum designed for graduating medical students is that our experiences have not been uniform. Since fourth year is comprised mostly of electives, we have all built different strengths and skills. Our last block of medical school is designed to smooth out any deficiencies but as a result, some lectures and small groups are basic for some people and new to others. I attended a small group on working with the difficult patient which was very enlightening because such experiences are common but we often forget to debrief about them. How do you deal with a patient who is demanding, demeaning, uncooperative, clingy, borderline, or unreasonable? Unfortunately, we all get these patients in the hospital, but we aren't trained well to handle them, and subsequently, they may get less-than-ideal care. One of the great psychiatry attendings came to facilitate the discussion because psychiatrists have the best formal training on personality disorders. I also chose small groups dealing with topics like inpatient diabetes management (converting outpatient regiments for inpatient ones, how to manage insulin when someone is not eating, etc), how to survive the first night of call, and ICU basics.
Outside of these small group sessions, I participated on a panel for the upcoming fourth year medical students about applying to preliminary residency programs. The anesthesia department also held a celebratory toast in honor of those who matched this year, inviting third and fourth years to come ask us questions.
Outside of these small group sessions, I participated on a panel for the upcoming fourth year medical students about applying to preliminary residency programs. The anesthesia department also held a celebratory toast in honor of those who matched this year, inviting third and fourth years to come ask us questions.
Subscribe to:
Posts (Atom)


